Epidemiology
- History: first described in 1936
- Prevalence: 3 per 100k in US
- Most common vasculitis to involve the lungs
- Represents 10% of all systemic vasculitides diagnosed
- Race: overwhelming predilection for caucasians
- Sex: M = F
- Mean Age of Onset: 40 y/o (15% of cases are <19 y/o)
Etiology
- Alpha-1 Antitrypsin Deficiency (see Alpha-1 Antitrypsin Deficiency)
- Due to the Strong Association Between c-ANCA Positive Vasculitis and A1AT Deficiency, It Has Been Suggested that All Wegener’s Granulomatosis Patients Be Tested for A1AT (Phenotyping or Genotyping May Be Required, Since A1AT is an Acute Phase Reactant Which Increases During Active Vasculitis)
Physiology
Necrotizing Vasculitis Involving Small Arteries and Veins
Airway Involvement
- xxxx
Pathologic Features
(histologic material usually obtained from OLB)
- Parenchymal Necrosis or Neutrophilic Microabscesses: geographic pattern
- Granulomatous Inflammation: although it is usually a mixed infiltrate of neutrophils, lymphocytes, plasma cells, eosoinophils, and histiocytes
- Small-Medium Arterial Necrotizing Vasculitis (although can involve capillaries and veins): vessel obstruction, bland infarcts
- Pulmonary Capillaritis: seen in about up to 33% of cases, but is an isolated finding in <3% of cases
- Neutrophilic Invasion of Alveolar Interstitium with Fibrinoid Necrosis: destroyed alveolar-capillary membrane (leakage of RBC and neutrophils into alveoli)
- Leukocytoclasis: neutrophils appear fragmented (nuclear dust accumulates in parenchyma)
- Hemosiderin-Laden Macrophages/Free hemosiderin in Interstitium: appear after acute bleed
- Type II Pneumocyte Hyperplasia/Organizing Pneumonia (organization of intra-alveolar hemorrhage)
- Mononuclear Cell Infiltration of Interstitium
- Small Thrombi in Capillaries and Venules
- Note: pulmonary HTN is rare in Wegener’s
- Pulmonary Capillaritis: seen in about up to 33% of cases, but is an isolated finding in <3% of cases
- Minor Histologic Criteria
- Organizing Pneumonia (70% of cases)
- Diffuse Alveolar Hemorrhage (10% of cases)
- Eosinophilia
- Bronchocentric Granulomatosis (1% of cases)
- Circulating Endothelial Cells: may be found in Wegener’s and microsocpic polyangiitis -> may serve as a marker for active ANCA-associated vasculitis
Diagnosis
Complete Blood Count (CBC) (see Complete Blood Count)
- Anemia (iron deficiency): usually present
- Leukocytosis
Erythrocytes Sedimentation Rate (ESR) (see procxx
- Usually markedly elevated
Urinalysis (see Urinalysis)
- Abnormal
Arterial Blood Gas (ABG) (see xxxxx)
- hypoxemia (with elevated A-a gradient)
- Serum Ig: elevated
Serology – ANA: variable – Anti-DNA: negative – RF: variable (may be mildly elevated) – C3/C4/CH50: normal – c-ANCA (cytoplasmic staining, typically directed against proteinase 3, PR3): positive (>1:20) in >90-95% of untreated active systemic Wegener’s Granulomatosis cases – However, c-ANCA is only positive in 60-65% of limited Wegener’s Granulomatosis cases – ANCA positivity declines with remission but is not sensitive enough to follow disease course – Anti-GBM: negative
Chest CT (see Chest Computed Tomography)
- Findings
- xxx
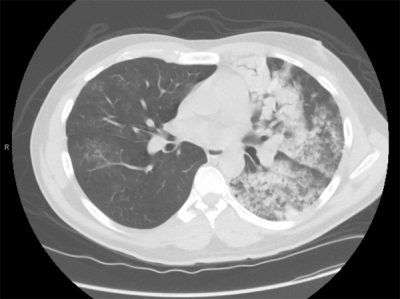
- Example: diffuse alveolar hemorrhage in a patient with Wegener’s granulomatosis -> note the ground glass infiltrates in the right lung and extensive alveolar filling in the left lung (alveolar hemorrhage was confirmed in the left lower lobe by bronchoscopy)
Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- DLCO: increased during DAH/decreased at other times
- Restriction (due to fibrosis) may be seen late
- Increased VD/VT ratio
Bronchoscopy (see Bronchoscopy)
- BAL with Diffuse Alveolar Hemorrhage: RBC’s, hemosiderin-laden macrophages (hemosiderin-laden macrophages indicate prior or recurrent alveolar hemorrhage)
Fluorodeoxyglucose-Positron Emission Tomography (FDG-PET) (see Fluorodeoxyglucose-Positron Emission Tomography)
- xxx
Video-Assisted Thoracoscopic Surgery (VATS) with Lung Biopsy (see xxxx)
- xxxx
- OLB (best diagnostic yield of any tissue for Wegener’s Granulomatosis)
- Tissue Ab staining: granular pattern or negative
Upper Airway Biopsy
- Diagnostic
Skin Biopsy (see xxxx)
- May be diagnostic
Renal Biopsy (see xxxx)
- Focal segmental necrotizing glomerulonephritis and crescents
- Usually not helpful in diagnosing this condition due to non-specific changes
Clinical Diagnostic Criteria (with >2 of these criteria, sensitivity is 88% and specificity is 92%)
- Nasal or Oral Inflammation
- Abnormal Chest X-Ray (CXR)
- Abnormal Urinary Sediment
- Granulomatous Inflammation on Biopsy
- Hemoptysis (see xxxx)
Limited Wegener’s Granulomatosis
- Systemic Disease without Glomerulonephritis
- Unclear if This is an Earlier Form of Disease or a Clinical Variant
Clinical Features
- General Comments
- Disease Course: symptoms are usually present for only days-weeks before presentation
Cardiovascular Manifestations
- General Comments: occur in 5-30% of cases
- Arrhythmias
- Arteritis
- Endocarditis (see Endocarditis)
- Myocarditis (see Myocarditis)
- Pericarditis (see Pericarditis)
Dermatologic Manifestations
- General Comments: occur in 45% of cases
- Leukocytoclastic Vasculitic Rash (splinter hemorrhages/palpable purpura): may be present
- Skin Nodules
- Ulcers (see xxxx)
- Vesicles (see xxxx)
Gastrointestinal Manifestations
General Comments
- Gastrointestinal Manifestations Occur in <10% of Cases
Intestinal Ischemia/Infarction (see Acute Mesenteric Ischemia)
- Epidemiology
- XXXX
Gastrointestinal Perforation
- Epidemiology
- XXXX
Ulcerative Lesions
- Epidemiology
- XXXX
Weight Loss (see Weight Loss)
- Epidemiology
- XXXX
Neurologic Manifestations (22%)
Fatigue (see Fatigue)
- Epidemiology
- XXXX
Peripheral Neuropathy (see xxxx)
- Epidemiology
- XXXX
Mononeuritis Multiplex (see xxxx)
- Epidemiology
- XXXX
Cranial Neuropathies
- Epidemiology
- XXXX
External Ophthalmoplegia
- Epidemiology
- XXXX
Seizures (see xxxx)
- Epidemiology
- XXXX
Cerebritis
- Epidemiology
- XXXX
Cerebrovascular Accident (CVA) (see xxxx)
- Epidemiology
- XXXX
Posterior Reversible Encephalopathy Syndrome (PRES) (see Posterior Reversible Encephalopathy Syndrome)
- Epidemiology
- XXXX
Ophthamlogic Manifestations (25-60%)
- Proptosis
- Uveitis
- Ocular Ulcers
- Conjunctivitis
- Scleritis
- Retinal and Optic Nerve Vasculitis
Pulmonary Manifestations
General Comments
- Parenchymal Abnormalities Occur in 45% of Cases on Initial Presentation
- Eventually, 85% of Cases Develop Parenchymal Abnormalities
Acute/Chronic Bronchiolitis (see Bronchiolitis)
- Epidemiology
- Less Common Clinical Presentation
Bronchiolitis Obliterans (BO) (see Bronchiolitis Obliterans)
- Epidemiology
- Less Common Clinical Presentation
Diffuse Alveolar Hemorrhage (DAH) (see Diffuse Alveolar Hemorrhage)
- Epidemiology
- Recurrent Diffuse Alveolar Hemorrhage Appears to Be More Common in ANCA-Associated Vasculitis than with Other Etiologies of Diffuse Alveolar Hemorrhage
- Diagnosis
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
- Alveolar infiltrates: during acute diffuse alveolar hemorrhage
- Intersitital infiltrates: after chronic or recurrent diffuse alveolar hemorrhage
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
- Clinical
- Chest Pain (see Chest Pain): may occur
- Cough (see Cough)
- Dyspnea (see Dyspnea)
- Hemoptysis (see xxxx)
- Occurs in 95% of Cases
- Due to Capillaritis
- May Occur on initial Presentation or in Established Disease
- May Be Absent on Initial Presentation in Some Cases, Even After Significant Bleeding
Endobronchial Ulcerating Lesions or Stenosis
- Epidemiology
- Tracheobronchial or Endobronchial Disease Occurs in 10-50% of Cases
- Diagnosis
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
- Post-Obstructive Atelectasis (see Atelectasis)
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
Interstitial Lung Disease (see Interstitial Lung Disease): less common presentation
- Epidemiology
- May occur after chronic or recurrent diffuse alveolar hemorrhage
Lipoid Pneumonia (see Lipoid Pneumonia)
- Epidemiology
- Less Common Clinical Presentation
Lung Nodules (see Lung Nodule or Mass)
- Epidemiology: occur in 31% of cases
- Diagnosis
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
- Approximately 80% of Cases Have <10 Nodules
- Cavitary Nodules Occur in 10% of Cases
- Absence of Calcification within Lung Lesions
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
Mediastinal Lypmhadenopathy (see Mediastinal Mass)
- Epidemiology
- Occurs in Only 2-15.7% of Cases
- Clinical
- Absence of Hilar Lymphadenopathy
- Massive Lymphadenopathy is Uncommon
Pleural Effusion/Thickening (see Pleural Effusion-Exudate)
- Diagnosis
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
- Pleural Effusion
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
Pneumonia-Like Picture (see Pneumonia)
- Epidemiology
- Pneumonia-Like Presentation Occurs in 63% of Cases
- Diagnosis
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
- Diffuse or Patchy Alveolar Infiltrates
- Chest X-Ray (CXR)/Chest Computed Tomography (CT) (see Chest X-Ray and Chest Computed Tomography)
Pulmonary Hypertension (see Pulmonary Hypertension)
- Epidemiology
- Pulmonary Hypertension is Rare
- Diagnosis
- Echocardiogram (see Echocardiogram)
- Useful to Diagnose Pulmonary Hypertension
- Echocardiogram (see Echocardiogram)
Renal Manifestations
General Comments
- Renal Manifestations Occur in 50-90% of Cases
Glomerulonephritis
- Epidemiology
- Approximately 80-90% of Patients Will Eventually Develop Renal Manifestations, But Only 40% Have Renal Symptoms on Initial Presentation)
Rheumatologic Manifestations
- General Comments: occur in 80% of cases
- Arthralgias (see Arthralgias)
- Myalgias (see Myalgias)
- Polyarthritis (see Arthritis)
Upper Airway Manifestations (75-90% of cases)
- Bony Destruction (may mimic Lethal Midline Granuloma, which involves only the nose and face)
- Nasal or Upper Airway Ulcers (see xxxx)
- Otitis (see xxxx)
- Rhinitis (see xxxx)
- Sinusitis (see xxxx): most common presenting symptom
- Subglottic Stenosis (23% of cases in one NIH series): may require tracheostomy
Other Manifestations
- Fever (see Fever)
- Malaise
- Nasolacrimal Duct Involvement
- Salivary Gland Involvement
Treatment
Induction in Mild Disease
Criteria for Mild Disease
- Absence of Active Glomerulonephritis
- Normal Creatinine
- No Red Blood Cell Casts
- No Proteinuria
- Absence of Organ-Threatening/Life-Threatening Manifestations
- Absence of Pulmonary Hemorrhage
- Absence of Cerebral Vasculitis
- Absence of Progressive Neuropathy
- Absence of Orbital Pseudotumor
- Absence of Gastrointestinal Bleeding
- Absence of Pericarditis
- Absence of Myocarditis
Regimens
- Corticosteroids + Methotrexate (see Corticosteroids and Methotrexate)
- Initial Therapy for Patients with Mild Extrarenal Disease and Little or No Renal Involvement
- Corticosteroids + Cyclophosphamide (Cytoxan) (see Corticosteroids and Cyclophosphamide)
- Alternative for Patients with Lack of Response or Progression on Methotrexate Therapy
- Adverse Effects
- Cyclophosphamide-Specific Side Effects (see Cyclophosphamide)
- Cystitis: occur in 12% of cyclophosphamide-treated patients
- Myelodysplastic Syndrome: occurs in 8% of cyclophosphamide-treated patients
- Solid Malignancy: occurs in 5% of cyclophosphamide-treated patients
- Infection
- Clinically-Important Infection: occurs in 10% of cyclophosphamide-treated patients (even in the absence of cyclophosphamide-induced leukopenia)
- Combined Corticosteroids + Cyclophosphamide Increase the Risk of Infection Over that of Cyclophosphamide Alone
- Cyclophosphamide-Specific Side Effects (see Cyclophosphamide)
- Corticosteroids + Rituximab (Rituxan) (see Corticosteroids and Rituximab)
- Alternative for Patients with Lack of Response or Progression on Methotrexate Therapy
- Clinical Efficacy
- Open-Label Rituximab Trial in Wegener’s Granulomatosis (Am J Respir Crit Care Med, 2006) [MEDLINE]
- Rituximab Was a Well-Tolerated and Effective Remission Induction Agent for Severe Refractory Wegener’s Granulomatosis
- RAVE-ITN Trial of Rituximab vs Cyclophosphamide for ANCA-Associated Vasculitis (Wegener’s Granulomatosis or Microscopic Polyangiitis) (NEJM, 2010) [MEDLINE]
- Rituximab Was Not Inferior to Daily Cyclophosphamide for Induction of Remission in Severe ANCA-Associated Vasculitis and May Be Superior in Relapsing Disease
- European Vasculitis Study Group-RITUXVAS Trial in ANCA-Associated Renal Vasculitis (NEJM, 2010) [MEDLINE]
- Rituximab Was Not Superior to Standard Intravenous Cyclophosphamide for Severe ANCA-Associated Vasculitis: sustained-remission rates were high in both groups
- No Difference in Adverse Events: rituximab-based regimen was not associated with reductions in early severe adverse events
- Multicenter Randomized Trial of Remission-Induction Regimens for ANCA-Associated Vasculitis (NEJM, 2013) [MEDLINE]
- Single Course of Rituximab was as Effective as Continuous Conventional Immunosuppressive Therapy for the Induction and Maintenance of Remission Over the Course of 18 mo
- Open-Label Rituximab Trial in Wegener’s Granulomatosis (Am J Respir Crit Care Med, 2006) [MEDLINE]
Pneumocystis Jirovecii Prophylaxis (see Pneumocystis Jirovecii)
- Indicated During Induction, Due to Risk of Infection (Am J Respir Crit Care Med, 1995) [MEDLINE]
Induction in Moderate-Severe Disease
Criteria for Moderate-Severe Disease
- Presence of Organ-Threatening/Life-Threatening Manifestations
- Pulmonary Hemorrhage
- Rapidly-Deteriorating Renal Function
Regimens
- General Comments: lack of disagreement about which of these regimens is preferred
- Corticosteroids + Cyclophosphamide (Cytoxan) (see Corticosteroids and Cyclophosphamide)
- Preferred Regimen in the Setting of Mechanical Ventilation or Cr >4 mg/dL, Since Rituximab Has Not Been Well-Studied in These Settings
- Cyclophosphamide: PO or IV
- Corticosteroids and Oral Cyclophosphamide Induce Remission in 85-90% of Cases, with Approximately 75% of Cases Achieving Complete Remission
- Most Remissions Occur Between 2-6 mo
- Adverse Effects
- Cyclophosphamide-Specific Side Effects (see Cyclophosphamide)
- Cystitis: occur in 12% of cyclophosphamide-treated patients
- Myelodysplastic Syndrome: occurs in 8% of cyclophosphamide-treated patients
- Solid Malignancy: occurs in 5% of cyclophosphamide-treated patients
- Infection
- Clinically-Important Infection: occurs in 10% of cyclophosphamide-treated patients (even in the absence of cyclophosphamide-induced leukopenia)
- Combined Corticosteroids + Cyclophosphamide Increase the Risk of Infection Over that of Cyclophosphamide Alone
- Cyclophosphamide-Specific Side Effects (see Cyclophosphamide)
- Corticosteroids + Rituximab (Rituxan) (see Corticosteroids and Rituximab)
- Preferred Regimen in Patients with Concerns About the Risk of Malignancy or Fertility
- Plasma Exchange (see Plasmapheresis and Plasma Exchange)
- Recommended as Add-On Therapy for the Following Indications
- Concurrent Anti-GBM Antibody Disease
- Cr >5.7 mg/dL
- Need for Hemodialysis (see Hemodialysis)
- Severe Active Renal Disease
- Severe Pulmonary Hemorrhage (see Diffuse Alveolar Hemorrhage)
- Rationale: plasma exchange removes ANCA
- Clinical Efficacy
- Retrospective Review of Plasmapheresis for Diffuse Alveolar Hemorrhage in Patients with Small Vessel Vasculitis (Am J Kidney Dis, 2003) [MEDLINE]
- Plasmapheresis with Immunosuppression is Effective in ANCA-Associated Small Vessel Vasculitis and Diffuse Alveolar Hemorrhage
- Randomized Trial of Plasma Exchange or High-Dose Methylprednisolone as Adjunctive Therapy in Severe Renal Vasculitis (J Am Soc Nephrol, 2007) [MEDLINE]
- As Compared to Intravenous Methylprednisolone, Plasma Exchange was Associated with a Decreased Risk in Progression to End-Stage Renal Disease at 12 mo
- Plasma Exchange Increased the Rate of Renal Recovery in ANCA-Associated Vasculitis with Renal Failure, as Compared to Intravenous Methylprednisolone
- No Difference in Mortality Rate Between the Groups
- PEXIVAS Trial is Currently in Process to Examine the Benefit of Plasma Exchange
- Retrospective Review of Plasmapheresis for Diffuse Alveolar Hemorrhage in Patients with Small Vessel Vasculitis (Am J Kidney Dis, 2003) [MEDLINE]
- Recommended as Add-On Therapy for the Following Indications
- Clinical Efficacy
- Open-Label Rituximab Trial in Wegener’s Granulomatosis (Am J Respir Crit Care Med, 2006) [MEDLINE]
- Rituximab Was a Well-Tolerated and Effective Remission Induction Agent for Severe Refractory Wegener’s Granulomatosis
- RAVE-ITN Trial of Rituximab vs Cyclophosphamide for ANCA-Associated Vasculitis (Wegener’s Granulomatosis or Microscopic Polyangiitis) (NEJM, 2010) [MEDLINE]
- Rituximab Was Not Inferior to Daily Cyclophosphamide for Induction of Remission in Severe ANCA-Associated Vasculitis and May Be Superior in Relapsing Disease
- European Vasculitis Study Group-RITUXVAS Trial in ANCA-Associated Renal Vasculitis (NEJM, 2010) [MEDLINE]
- Rituximab Was Not Superior to Standard Intravenous Cyclophosphamide for Severe ANCA-Associated Vasculitis: sustained-remission rates were high in both groups
- No Difference in Adverse Events: rituximab-based regimen was not associated with reductions in early severe adverse events
- Multicenter Randomized Trial of Remission-Induction Regimens for ANCA-Associated Vasculitis (NEJM, 2013) [MEDLINE]
- Single Course of Rituximab was as Effective as Continuous Conventional Immunosuppressive Therapy for the Induction and Maintenance of Remission Over the Course of 18 mo
- Open-Label Rituximab Trial in Wegener’s Granulomatosis (Am J Respir Crit Care Med, 2006) [MEDLINE]
Pneumocystis Jirovecii Prophylaxis (see Pneumocystis Jirovecii)
- Indicated During Induction, Due to Risk of Infection (Am J Respir Crit Care Med, 1995) [MEDLINE]
Maintenance Therapy
- Azathioprine (Imuran) (see Azathioprine)
- Methotrexate (see Methotrexate)
- Mycophenolate Mofetil (Cellcept) (see Mycophenolate Mofetil)
- Rituximab (Rituxan) (see Anti-CD20 Therapy)
Relapse
- Prevalance of Relapse
- 50% of all ANCA-associated vasculitis patients have at least one relapse, despite active treatment
- Relapse occurs in 40-65% of Wegener’s Granulomatosis cases (in contrast, relapse occurs in 25-33% of Microscopic Polyangiitis cases and 15-25% of Churg-Strauss cases)
- Site of Relapse: may be in an initially affected organ or in a new organ
- Treatment of Relapse: repeat induction
Disease Markers to Follow
- Erythrocyte Sedimentation Rate (ESR)
- ANCA
- DLCO
- Urinalysis
Prognosis
- 5-Year Survival: 75%
- Survival: months-years without treatment
- Causes of Death: cardiac disease, infection, renal failure, malignancy
- Predictors of Poor Outcome: advanced age, lack of otolaryngology clinician involvement, more severe renal disease, pulmonary involvement (especially with diffuse alveolar hemorrhage), hypoalbuminemia, high level of anti-PR3 (c-ANCA) positivity
- Better prognosis with limited Wegener’s
References
General
- Cardiac involvement in Wegener’s granulomatosis. Br Heart J. 1995 February; 73(2): 110–115
- Neurological involvement in Wegener’s granulomatosis: an analysis of 324 consecutive patients at the Mayo Clinic. Ann Neurol. Jan 1993;33(1):4-9
- An unusual presentation of relapsing Wegener’s granulomatosis. Nephrol. Dial. Transplant. (2001) 16 (7): 1511-1512
- Severe Intestinal Involvement in Wegener’s Granulomatosis: Report of Two cases and Review of the Literature. British Journal of Rheumatology 1998;37:387–390
- Pulmonary renal syndrome: a 4-year, single-center experience. Am J Kidney Dis. 2002 Jan;39(1):42-7 [MEDLINE]
Classification
- Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994;37(2):187 [MEDLINE]
- 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1 [MEDLINE]
Treatment
- Pneumocystis carinii pneumonia: a major complication of immunosuppressive therapy in patients with Wegener’s granulomatosis. Am J Respir Crit Care Med. 1995 Mar;151(3 Pt 1):795-9 [MEDLINE]
- Plasmapheresis therapy for diffuse alveolar hemorrhage in patients with small-vessel vasculitis. Am J Kidney Dis. 2003 Dec;42(6):1149-53 [MEDLINE]
- Rituximab for refractory Wegener’s granulomatosis: report of a prospective open-label pilot trial. Am J Respir Crit Care Med 2006;173:180-187 [MEDLINE]
- Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol. 2007 Jul;18(7):2180-8. Epub 2007 Jun 20 [MEDLINE]
- RAVE-ITN Research Group. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010 Jul 15;363(3):221-32. doi: 10.1056/NEJMoa0909905 [MEDLINE]
- European Vasculitis Study Group. Rituximab versus Cyclophosphamide for ANCA-Associated Vasculitis. N Engl J Med 2010; 363:221-232 [MEDLINE]
- RAVE-ITN Research Group. Efficacy of remission-induction regimens for ANCA-associated vasculitis. N Engl J Med 2013;369(36):417-427 [MEDLINE]
- Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014;371(19):1771 [MEDLINE]
- Plasmapheresis therapy for diffuse alveolar hemorrhage in patients with small-vessel vasculitis. Am J Kidney Dis. 2003 Dec;42(6):1149-53 [MEDLINE]
- Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol. 2007 Jul;18(7):2180-8. Epub 2007 Jun 20 [MEDLINE]