Epidemiology
General
Prevalence of Hypertension (Blood Pressure ≥130/80) in Adults (Age 18-80 y/o) in the United States (Data from 2017-2020) (Circulation, 2025) MEDLINE]
General Comments
- Prevalence of Hypertension Varies with the Following Factors
- Age
- Trends in Blood Pressure with Aging
- Population Systolic Blood Pressure Levels Increase Steadily to the End of Life
- Population Diastolic Blood Pressure Levels Increase Until the 5th Decade of Life, Plateau for a Decade, Then Decrease Thereafter
- Trends in Blood Pressure with Aging
- Sex
- Ethnicity
- Age
Male and Female Combined
- Overall: 46.7%
Male
- Overall: 49.5%
- Age 18-29 y/o: 20.3%
- Age 30-44 y/o: 39.6%
- Age 45-59 y/o: 57.4%
- Age 60-74 y/o: 70.7%
- Age 75-80 y/o: 83.7%
- Non-Hispanic White: 47.0%
- Non-Hispanic Black: 56.8%
- Non-Hispanic Asian: 49.8%
- Hispanic: 50.4%
- Other: 50.7%
Female
- Overall: 43.9%
- Age 18-29 y/o: 9.0%
- Age 30-44 y/o: 23.7%
- Age 45-59 y/o: 52.5%
- Age 60-74 y/o: 71.4%
- Age 75-80 y/o: 84.8%
- Non-Hispanic White: 39.0%
- Non-Hispanic Black: 56.7%
- Non-Hispanic Asian: 39.1%
- Hispanic: 36.3%
- Other: 47.9%
Coexistence of Hypertension and Other Comorbid Conditions
Hypertension Frequently Co-Occurs with Other Cardiovascular Disease Risk Factors
- Approximately 16.6% of Adults with Hypertension are Current Smokers (see Tobacco)
- Approximately 72.6% of Adults with Hypertension are Overweight/Obese (see Obesity)
- Approximately 12.3% of Adults with Hypertension Have Diabetes Mellitus (see Diabetes Mellitus)
- Approximately 13.4% of Adults with Hypertension Have Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- In All Adults with Hypertension, Screening/Management of Other Modifiable Cardiovascular Disease Risk Factors are Recommended (Class of Recommendation: I, Level of Evidence: B-NR
- Modifiable Risk Factors
- Current Cigarette Smoking/Secondhand Smoking (see Tobacco)
- Diabetes Mellitus (DM) (see Diabetes Mellitus)
- Hyperlipidemia (see Hyperlipidemia)
- Overweight/Obesity (see Obesity)
- Physical Inactivity/Low Fitness Level
- Unhealthy Diet
- Relatively Fixed Risk Factors
- Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Family History of Cardiovascular Disease
- Low Socioeconomic/Educational Status
- Male Sex
- Older Age
- Obstructive Sleep Apnea (OSA) (see Obstructive Sleep Apnea)
- Psychosocial Stress
- Modifiable Risk Factors
Risk Factors for Hospitalization for Hypertension (Hypertension, 2024) [MEDLINE]
- Low Socioeconomic Status
- Poor Compliance with Antihypertensive Medication Regimen
- Residence in Low Income Area
- Underinsurance/Lack of Health Insurance
Hypertension in the Emergency Department (ED) Setting
- In 2012, Hypertension was the Primary Diagnosis in Over 1 Million Emergency Department Visits (with Approximately 23% of These Resulting in Hospitalization) (Hypertension, 2024) [MEDLINE]
Hypertension in the Inpatient Setting
Clinical Data
- Systematic Review of Studies of Hypertension in the Inpatient Setting (J Hosp Med, 2011) [MEDLINE]: n = 9 studies
- Inpatient Hypertension (with or without Target-Organ Damage) is Present in Up 50.5-72% of Inpatients
- Approximately 37-77% of Hypertensive Patients Remained Hypertensive at the Time of Discharge
- Most Patients with Inpatient Hypertension Continued to Have Elevated Blood Pressures at the Time of Outpatient Follow-Up
- Study of Hypertension in Adults in the Inpatient Setting (JAMA Intern Med, 2021) MEDLINE]: n = 22,834 patients admitted to a medicine service for non-cardiac diagnoses
- Systolic Blood Pressure (Defined >140 mm Hg) was Present at Least One Time in 78% of Patients
- Multi-Hospital Retrospective Cohort Study of Hypertension in the Inpatient Setting (J Clin Hypertens-Greenwich, 2022) [MEDLINE]: n = 224,265 hospitalized adults (admitted for reasons other than hypertension)
- Approximately 10% of Patients Developed Severe Hypertension (of Which 40% were Treated)
Risk Factors for Asymptomatic Elevated Inpatient Blood Pressure and/or Hypertensive Emergencies (Hypertension, 2024) [MEDLINE]
- Black Race
- Cardiovascular Disease
- Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Diabetes Mellitus (see Diabetes Mellitus)
- Older Age
Hypertensive Emergencies
Clinical Data
- Data from the Nationwide Emergency Department Sample from 2006-2013 Indicated that Hypertensive Emergencies Occurred in Approximately 2/1,000 Adult Emergency Department Visits Overall (and in 6/1,000- Emergency Department Visits in Patients with a Prior Diagnosis of Hypertension) (Hypertension, 2024) [MEDLINE]
- Systematic Review and Meta-Analysis (8 Studies) of Hypertensive Urgency/Emergency Patients Presenting to the Emergency Department (J Hypertens, 2020) [MEDLINE]
- Prevalence of Hypertensive Urgency: 0.9%
- Prevalence of Hypertensive Emergency: 0.3%
- The Rate of Hypertensive Emergencies Has Increased Over the Past 20 yrs (Hypertension, 2024) [MEDLINE]
- However, Over that Period of Time, Hypertensive Emergency Mortality Rates Have Decreased (Range from 0.2-11%)
Risk Factors for Asymptomatic Elevated Inpatient Blood Pressure and/or Hypertensive Emergencies (Hypertension, 2024) [MEDLINE]
- Black Race
- Cardiovascular Disease
- Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Diabetes Mellitus (see Diabetes Mellitus)
- Older Age
Etiology/Risk Factors (Hypertension, 2018) [MEDLINE]
General Comments
Primary vs Secondary Hypertension
- Secondary Hypertension Can Be Identified in Approximately 5-25% of Adult Patients with Hypertension (Circulation, 2025) MEDLINE]
- If a Secondary Etiology Can Be Diagnosed and Treated, Patient with Secondary Hypertension May Experience a Marked Improvement in Blood Pressure Control with a Resulting Decrease in Cardiovascular Disease Risk
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- In Adults with Hypertension, Screening for Specific Types of Secondary Hypertension is Recommended When Clinical Suspicion is Present to Increase Rates of Detection, Diagnosis, and Specific Targeted Therapy (Class of Recommendation: 1; Level of Evidence: C-EO)
- In Adults with Resistant Hypertension, Screening for Primary Aldosteronism is Recommended (Regardless of Whether Hypokalemia is Present) to Increase Rates of Detection, Diagnosis, and Specific Targeted Therapy (Class of Recommendation: 1; Level of Evidence: B-NR)
- In Adults Who Have a Positive Screening Test for a Type of Secondary Hypertension, Referral to a Clinician Who Has Expertise in that Type of Hypertension is Reasonable for Diagnostic Confirmation and Treatment (Class of Recommendation: 2a; Level of Evidence: C-EO)
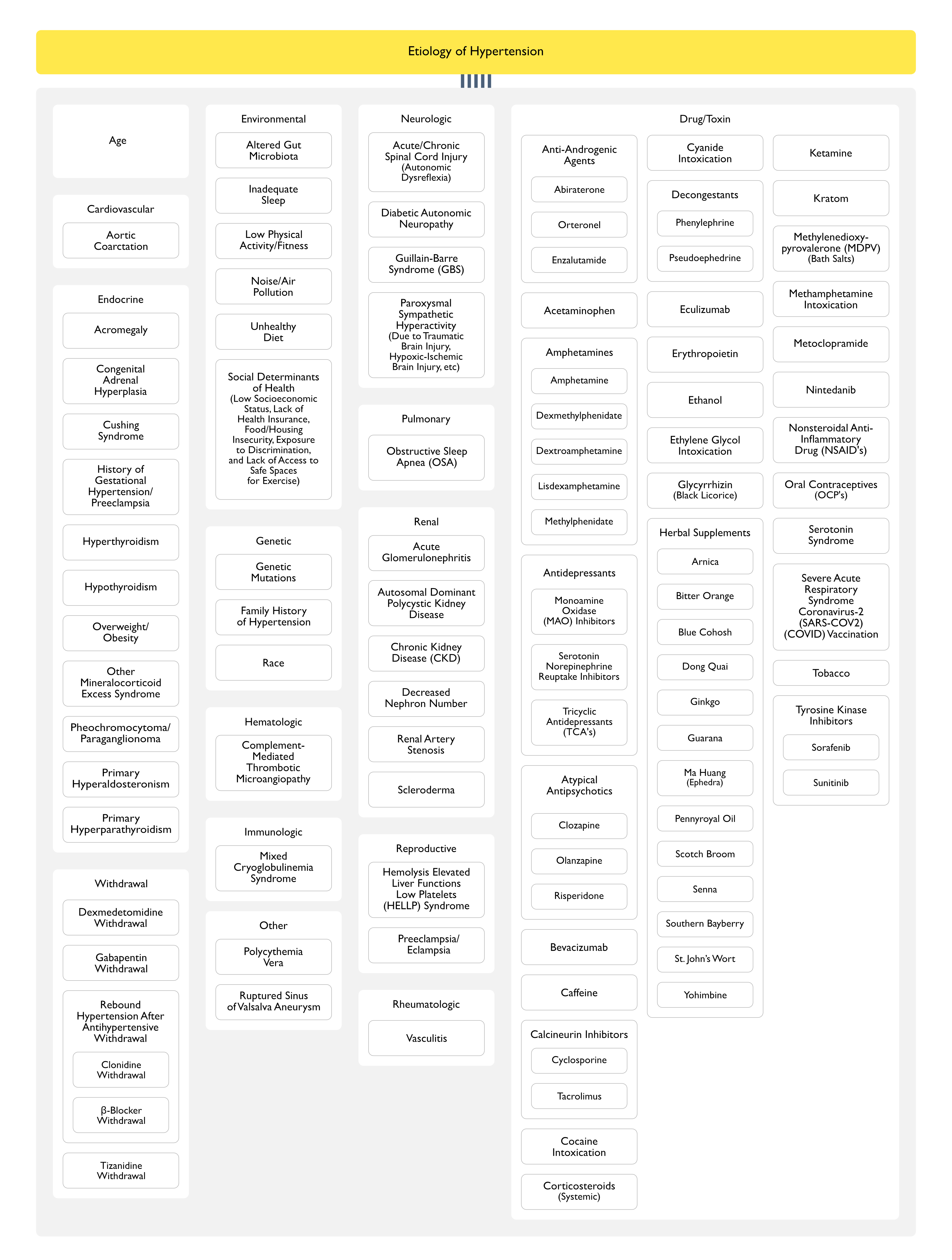
Age
- Epidemiology
- Advancing Age is Associated with Increased Blood Pressure (Especially Increased Systolic Blood Pressure), and an Increased Incidence of Hypertension
Cardiovascular
Aortic Coarctation (see Aortic Coarctation)
- Epidemiology
- Usually Diagnosed in Patient <30 y/o
- Diagnosis
- Echocardiogram (see Echocardiogram)
- Thoracic/Abdominal Computed Tomography Angiogram (CT)
- Thoracic/Abdominal Magnetic Resonance Angiogram (MRA)
- Clinical
- Abdominal bruit
- Absent Femoral Pulses
- Continuous Murmur Over Back/Chest
- Higher Blood Pressure in Upper Extremities than in Lower Extremities
Endocrine
Acromegaly (see Acromegaly)
- Epidemiology
- Acromegaly is a Rare Etiology of Secondary Hypertension (Circulation, 2025) MEDLINE]
- Diagnosis
- Brain Magnetic Resonance Imaging (MRI) (see Brain Magnetic Resonance Imaging)
- Elevated Age/Sex-Matched IGF-1 Level
- Serum Growth Hormone ≥1 ng/mL During Oral Glucose Load
- Clinical
- Acral Features
- Diabetes Mellitus (see Diabetes Mellitus)
- Enlarging Shoe/Glove/Hat Size
- Frontal Bossing
- Headache (see Headache)
- Visual Disturbances
Congenital Adrenal Hyperplasia (CAH) (see Congenital Adrenal Hyperplasia)
- Diagnosis
- Low/Normal Aldosterone and Renin
- 11-β-Hydroxylase Deficiency
- Decreased Cortisol and Corticosterone
- Increased 11-Deoxycortisol, 11-Deoxycorticosterone (DOC), Androstenedione, and Testosterone
- 17-α-Hydroxylase Deficiency
- Decreased Androgens and Estrogens
- Increased 11-Deoxycorticosterone (DOC), Corticosterone, and 18-Hydroxycorticosterone
- Clinical
- Hypertension
- Hypokalemia (see Hypokalemia)
- Virilization
- 11-β-Hydroxylase Deficiency
- Incomplete Masculinization in Males/Primary Amenorrhea in Females
- 17-α-Hydroxylase Deficiency
Cushing Syndrome (see Cushing Syndrome)
- Epidemiology
- Cushing Syndrome Accounts for <0.1% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Diagnosis
- 24 hr Urinary Free Cortisol Excretion (Preferably Multiple)
- Midnight Salivary Cortisol
- Overnight Dexamethasone Suppression Test (see Dexamethasone Suppression Test)
- Clinical
- “Buffalo Hump (Dorsal Fat Pad)
- Central Obesity (see Obesity)
- Depression (see Depression)
- Dorsal/Supraclavicular Fat Pads
- Easy Bruisability
- Hirsutism (see Hirsutism)
- Hyperglycemia (see Hyperglycemia)
- “Moon Face”
- Proximal Muscle Weakness
- Rapid Weight Gain (Especially with Central Distribution) (see Weight Gain)
- Supraclavicular Fat Pads
- Wide (1 cm) Violaceous Striae (see Striae)
History of Gestational Hypertension/Preeclampsia (see Preeclampsia and Eclampsia)
- Epidemiology
- Females with a History of High Blood Pressure During Pregnancy are More Likely to Develop Sustained Hypertension Later in Life (Even if the Blood Pressure Normalizes Initially After Delivery)
Hyperthyroidism (see Hyperthyroidism)
- Epidemiology
- Hyperthyroidism Accounts for <1% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Diagnosis
- Radioactive Iodine Uptake and Scan
- Serum Free T4
- Serum Thyroid Stimulating Hormone (TSH) (see Serum Thyroid Stimulating Hormone)
- Clinical
- Anxiety (see Anxiety)
- Diarrhea (see Diarrhea)
- Heat Intolerance
- Insomnia (see Insomnia)
- Lid Lag
- Palpitations (see Palpitations)
- Proximal Muscle Weakness
- Tremor (see Tremor)
- Warm, Moist Skin
- Weight Loss (see Weight Loss)
Hypothyroidism (see Hypothyroidism)
- Epidemiology
- Hypothyroidism Accounts for <1% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Diagnosis
- Serum Free T4
- Serum Thyroid Stimulating Hormone (TSH) (see Serum Thyroid Stimulating Hormone)
- Clinical
- Cold Intolerance
- Constipation (see Constipation)
- Delayed Ankle Reflex
- Dry, Coarse, Cold Skin
- Goiter (see Goiter)
- Hoarseness (see Hoarseness)
- Periorbital Edema/Puffiness
- Slow Movement
- Weight Gain (see Weight Gain)
Overweight/Obesity (see Obesity)
- Epidemiology
- Diagnosis
- Recommendations-2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (Hypertension, 2018) [MEDLINE]
- Weight Loss is Recommended to Decrease Blood Pressure in Adults with Hypertension Who are Overweight/Obese (Class of Recommendation: I, Level of Evidence: A)
- Recommendations-2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (Hypertension, 2018) [MEDLINE]
Other Mineralocorticoid Excess Syndrome (Other than Primary Aldosteronism)
- Epidemiology
- Other Mineralocorticoid Excess Syndromes are a Rare Etiology of Secondary Hypertension (Circulation, 2025) MEDLINE]
- Etiology
- Deoxycorticosterone-Producing Adrenal Tumor
- Genetic Syndrome of Apparent Mineralocorticoid Excess: rare
- Diagnosis
- Decreased Serum Aldosterone
- Decreased Serum Renin
- Genetic Testing
- Urinary Cortisol Metabolites
- Clinical
- Early-Onset/Resistant Hypertension
- Hyperkalemia (see Hyperkalemia)
- Hypokalemia (see Hypokalemia)
- May be Severe Enough to Cause Arrhythmias
Pheochromocytoma/Paraganglionoma (see Pheochromocytoma)
- Epidemiology
- Pheochromocytoma/Paraganglionoma Account for <0.6% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Diagnosis
- Abdominal/Pelvic Computed Tomography (CT) or Abdominal/Pelvic Magnetic Resonance Imaging (MRI) (see Abdominal-Pelvic Computed Tomography or Abdominal/Pelvic Magnetic Resonance Imaging)
- Adrenal Mass (see Adrenal Mass)
- Plasma Metanephrines (see xxxx)
- Urinary Fractionated Metanephrines (24 hr) (see xxxx)
- Abdominal/Pelvic Computed Tomography (CT) or Abdominal/Pelvic Magnetic Resonance Imaging (MRI) (see Abdominal-Pelvic Computed Tomography or Abdominal/Pelvic Magnetic Resonance Imaging)
- Clinical
- Adrenal Mass (see Adrenal Mass)
- Diaphoresis (see Diaphoresis)
- Headache (see Headache)
- Episodic Pallor (see Pallor)
- Episodic Dizziness (see Dizziness)
- Palpitations (see Palpitations)
- Paroxysmal/Labile Hypertension
- Piloerection (see Piloerection)
- Resistant Hypertension
Primary Hyperaldosteronism (see Hyperaldosteronism)
- Epidemiology
- Primary Hyperaldosteronism Accounts for Approximately 5-25% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Physiology
- Patients with Primary Hyperaldosteronism are at Greater Risk for Target Organ Damage (Heart Failure, Stroke, Coronary Artery Disease, Atrial Fibrillation, Chronic Kidney Disease, etc) than Those with Primary Hypertension Due to the Toxic Tissue Effects of Aldosterone (Even When Adjusted for Degree of Hypertension(
- Diagnosis
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- In Adults with Hypertension, Screening for Primary Hyperaldosteronism is Recommended in the Presence of Any of the Following Conditions to Increase Rates of Detection, Diagnosis, and Specific Targeted Therapy (Class of Recommendation: I; Level of Evidence: C-EO)
- Family History of Early-Onset Hypertension
- Hypokalemia (Spontaneous or Diuretic Induced) (see Hypokalemia)
- Incidentally Discovered Adrenal Mass (see Adrenal Mass)
- Resistant Hypertension (Regardless of Whether Hypokalemia is Present)
- Obstructive Sleep Apnea (OSA) (see Obstructive Sleep Apnea)
- Stroke at a Young Age (<40 y/o) (see Ischemic Cerebrovascular Accident)
- In Adults with Stage 2 Hypertension, Screening for Primary Hyperaldosteronism May Be Considered to Increase Rates of Detection, Diagnosis, and Specific Targeted Therapy (Class of Recommendation: 2b; Level of Evidence: C-EO)
- In Adults with an Indication for Screening for Primary Hyperaldosteronism, Use of Plasma Aldosterone, Renin Activity, and the Plasma Aldosterone/Renin Activity Ratio is Recommended for initial screening to assess if There is Biochemical Evidence of Primary Hyperaldosteronism (Class of Recommendation: 1; Level of Evidence: C-LD)
- In Adults with an Indication for Screening for Primary Hyperaldosteronism, it is Recommended to Continue Most Antihypertensives (Other than Mineralocorticoid Receptor Antagonists) Prior to Initial Screening to Minimize Barriers to or Delays in Screening (Class of Recommendation: 1; Level of Evidence: C-EO)
- In Adults with Hypertension and a Positive Screening Test for Primary Hyperaldosteronism or Continued Suspicion for Primary Hyperaldosteronism Based on Suppressed Plasma Renin or Disproportionate Target Organ Damage, Referral to a Hypertension Specialist or Endocrinologist is Recommended for Further Evaluation and Treatment (Class of Recommendation: 1; Level of Evidence: C-EO)
- In Adults with Hypertension, Screening for Primary Hyperaldosteronism is Recommended in the Presence of Any of the Following Conditions to Increase Rates of Detection, Diagnosis, and Specific Targeted Therapy (Class of Recommendation: I; Level of Evidence: C-EO)
- Plasma Aldosterone/Renin Ratio Under Standardized Conditions (Correction of Hypokalemia and Withdrawal of Aldosterone Antagonists for 4–6 wks)
- Oral Sodium Loading Test (with 24 hr Urine Aldosterone)
- Intravenous Saline Infusion Test with Plasma Aldosterone at 4 hrs of Infusion
- Adrenal Computed Tomography (CT) (see Abdominal Computed Tomography)
- Adrenal Mass (see Adrenal Mass)
- Adrenal Vein Sampling
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- Clinical
- Adrenal Mass (see Adrenal Mass)
- Early-Onset/Resistant Hypertension
- Early-Onset Stroke (see Ischemic Cerebrovascular Accident)
- Hypokalemia (see Hypokalemia)
- Either Spontaneous or Diuretic-Induced
- May be Severe Enough to Induce Arrhythmias (Especially Atrial Fibrillation) (see Atrial Fibrillation)
- Muscle Cramps/Weakness (see Muscle Cramps)
Primary Hyperparathyroidism (see Primary Hyperparathyroidism)
- Epidemiology
- Primary Hyperparathyroidism is a Rare Etiology of Secondary Hypertension (Circulation, 2025) MEDLINE]
- Diagnosis
- Serum Parathyroid Hormone (PTH) (see Serum Parathyroid Hormone)
- Clinical
- Effects of Hypercalcemia (see Hypercalcemia)
- Abdominal Pain (see Abdominal Pain)
- Anorexia (see Anorexia)
- Arrhythmias
- Atrioventricular Heart Blocks
- Confusion/Delirium (see Delirium)
- Constipation (see Weakness)
- Hypertension
- Nausea/Vomiting (see Nausea and Vomiting)
- Polydipsia (see Polydipsia)
- Polyuria (see Polyuria)
- Shortened QT Interval (see Shortened QT Interval)
- Sinus Bradycardia (see Sinus Bradycardia)
- Effects of Increased Parathyroid Hormone (PTH)
- Anemia (see Anemia)
- Bone Disease
- Hyperuricemia/Gout (see Hyperuricemia and Gout)
- Hypomagnesemia (see Hypomagnesemia)
- Hypophosphatemia (see Hypophosphatemia)
- Increased Calcitriol
- Nephrolithiasis (see Nephrolithiasis)
- Proximal Renal Tubular Acidosis (RTA) (see Metabolic Acidosis-Normal Anion Gap)
- Symptoms/Signs of Hypercalcemia (see Hypercalcemia)
- Effects of Hypercalcemia (see Hypercalcemia)
Environmental
Altered Gut Microbiota
- Demonstrated as a Risk Factor in Animal Models
Inadequate Sleep
- Short Sleep Duration (<7 hrs/Night) is Associated with a Higher Risk of Hypertension
- increasing Sleep Duration May Decrease Blood Pressure
Low Physical Activity/Fitness
- There is an Inverse Relationship Between Physical Activity/Physical Fitness and Hypertension
- Exercise (Aerobic, Dynamic Resistance, and Isometric Resistance) is Effective in Decreasing Blood Pressure
Noise/Air Pollution
- Exposure to Noise/Air Pollution Increases Blood Pressure
- Exposure to Noise/Air Pollution May Be an Important Contributor to Disparities in Hypertension Prevalence and Control
Unhealthy Diet
- Excess Dietary Sodium Intake
- Excess Sodium Intake is Positively Associated with Blood Pressure in Migrant, Cross-Sectional, and Prospective Cohort Studies
- Excess Sodium Intake Accounts for Much of the Age-Related Increase in Blood Pressure
- Insufficient Dietary Intake of Potassium, Calcium, Magnesium, Protein (Especially from Vegetables), fiber, and Fish Fats
- Potassium Intake is Inversely rRelated to Blood Pressure in Migrant, Cross-Sectional, and Prospective Cohort Studies
- Overweight/Obesity (see Obesity)
Social Determinants of Health
- Social Determinants of Health (Low Socioeconomic Status, Lack of Health Insurance, Food/Housing Insecurity, Exposure to Discrimination, and Lack of Access to Safe Spaces for Exercise) May Underlie Several of the Above Risk Factors for the Development of Hypertension (Such as Obesity, Poor Diet, Physical Inactivity, etc)* Social Factors Likely Account for a Large Part of the Observed Racial Disparities in Hypertension
Genetic
Hypertension is a Complex Polygenic Disorder in Which Many Genes or Gene Combinations Influence Blood Pressure
- Although Several Monogenic Forms of Hypertension Have Been Identified (Such as Glucocorticoid-Remediable Aldosteronism, Liddle’s Syndrome, Gordon’s Syndrome) in Which Single-Gene Mutations Fully Account for the Pathophysiology of Hypertension, These Disorders are Rare
- Known Genetic Variants Contributing to Hypertension Include >25 Rare Mutations and 120 Single-Nucleotide Polymorphisms
Family History of Hypertension
- Hypertension is Approximately 2x as Common in Patients Who Have 1-2 Hypertensive Parents
- Multiple Epidemiologic Studies Suggest that Genetic Factors Account for Approximately 30% of the Variation in Blood Pressure in Various Studied Populations (Lancet, 2003) [MEDLINE] (Arch Intern Med, 2008) [MEDLINE]
Race
- Features of Hypertension in Black Patients
- Higher Incidence of Hypertension
- Hypertension Occurring Earlier in Life
- Hypertension Tending to Be More Severe
- Hypertension Association with Greater Target-Organ Damage
Hematologic
Complement-Mediated Thrombotic Microangiopathy
- Epidemiology
- New/Worsening Hypertension is Common in Complement-Mediated Thrombotic Microangiopathy (Occurring in 8-54% of Cases) (see xxxx)
- Occurrence of Hypertension and Thrombotic Microangiopathy Together Should Especially Raise Suspicion if the Patient is Younger, Has a Poor Response to Antihypertensive Therapy, or if the Thrombotic Microangiopathy Does Not Improve with Antihypertensive Therapy Alone (Clin J Am Soc Nephrol, 2010) [MEDLINE] (Haematologica, 2019) [MEDLINE] (Hypertension, 2020) [MEDLINE]
- New/Worsening Hypertension is Common in Complement-Mediated Thrombotic Microangiopathy (Occurring in 8-54% of Cases) (see xxxx)
- Clinical
- Acute Kidney Injury (AKA) (see Acute Kidney Injury)
- Variably Occurs
- Microangiopathic Hemolytic Anemia (MAHA) (see Hemolytic Anemia)
- Thrombocytopenia (see Thrombocytopenia)
- Acute Kidney Injury (AKA) (see Acute Kidney Injury)
Immunologic
Mixed Cryoglobulinemia Syndrome (MCS) (see Cryoglobulinemia)
- Renal Clinical Presentations: similar in both type II and type III mixed cryoglobulinemia
- Acute Glomerulonephritis (see Glomerular Disease)
- Acute Kidney Injury (AKI) (see Acute Kidney Injury): 9% of cases
- Chronic Kidney Disease (CKD) without Significant Urinalysis Abnormalities (see Chronic Kidney Disease): 13% of cases
- Hypertension (Which May Be Severe): 65% of cases
- Microscopic Hematuria with Subnephrotic Proteinuria and with/without Chronic Kidney Disease (CKD) (see xxxx): 41% of cases
- Nephrotic Syndrome with/without Chronic Kidney Disease (CKD) (see Chronic Kidney Disease): 22% of cases
Neurologic
Acute/Chronic Spinal Cord Injury
- Epidemiology
- Acute Spinal Cord Injury May Manifest Autonomic Dysreflexia (see Acute Spinal Cord Injury)
- Chronic Spinal Cord Injury May Manifest Autonomic Dysreflexia (see Chronic Spinal Cord Injury)
- Autonomic Dysreflexia
- Autonomic Dysreflexia is a syndrome of acute autonomic instability that occurs in patients with cervical or high thoracic spinal cord injuries (above the T6 level)
- The Most Common precipitant of acute episodes is bladder distension; it may also occur after rectal distension, urologic or rectal procedures, or any painful stimuli [38]
- Common clinical features include sweating of the forehead or generalized sweating along with headache, gooseflesh, cutaneous vasodilation, increased muscle spasticity, an acute rise in blood pressure, and a desire to void
- This distinctive symptom constellation in the context of a patient with a spinal cord injury is not easily confused with other causes of sweating spells [39]
- Autonomic Dysreflexia is a syndrome of acute autonomic instability that occurs in patients with cervical or high thoracic spinal cord injuries (above the T6 level)
Diabetic Autonomic Neuropathy (see Diabetes Mellitus)
- Epidemiology
- Supine Hypertension
- Due to Loss of Diurnal Blood Pressure Variation
- Supine Hypertension
Guillain-Barre Syndrome (GBS) (see Guillain-Barre Syndrome)
- Epidemiology
- Paroxysmal Hypertension Occurs in 24% of Cases (Semin Neurol, 1984)
- Sustained Hypertension Occurs in 3% of Cases (Semin Neurol, 1984)
Paroxysmal Sympathetic Hyperactivity (PSH) (see Paroxysmal Sympathetic Hyperactivity)
- Epidemiology
- Paroxysmal Sympathetic Hyperactivity (PSH) is Most Commonly Associated with the Following
- Hypoxic-Ischemic Brain Injury (see Hypoxic-Ischemic Brain Injury)
- Traumatic Brain Injury (TBI) (see Traumatic Brain Injury)
- Paroxysmal Sympathetic Hyperactivity (PSH) is Most Commonly Associated with the Following
- Clinical
- Hypertension
- Sinus Tachycardia (see Sinus Tachycardia)
- Hyperventilation/Tachypnea/Respiratory Alkalosis (see Hyperventilation, Tachypnea, and Respiratory Alkalosis)
Pulmonary
Obstructive Sleep Apnea (OSA) (see Obstructive Sleep Apnea)
- Epidemiology
- Obstructive Sleep Apnea (OSA) Accounts for Approximately 25-50% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Diagnosis
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- In Adults with Hypertension and Obstructive Sleep Apnea (OSA) Who are Overweight/Obese, Weight Loss Interventions When Combined with Continuous Positive Airway Pressure (CPAP) Treatment Can Be Effective in Reducing Systolic Blood Pressure (Class of Recommendation: 2a, Level of Evidence: B-R)
- In Adults with Resistant Hypertension and Moderate-to-Severe Obstructive Sleep Apnea (OSA), Continued Positive Airway Pressure (CPAP) Treatment Can Be Useful in Reducing Blood Pressure (Class of Recommendation: 2a, Level of Evidence: B-R)
- Berlin Questionnaire
- Overnight Oximetry
- Polysomnogram (see Polysomnogram)
- STOP-BANG Questionnaire
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- Clinical
- Choking During Sleep
- Excessive Daytime Somnolence (EDS) (see Excessive Daytime Somnolence)
- Fitful Sleep
- Large Neck Circumference
- Male: >17 in
- Female: >16 in
- Loss of Normal Nocturnal Decrease in Blood Pressure
- Mallampati Class 3-4
- Obesity (see Obesity)
- Resistant Hypertension
- Respiratory Pauses During Sleep
- Snoring (see Snoring)
Renal
Acute Glomerulonephritis
- Epidemiology
- Patients with Acute Glomerular Disease (Such as Poststreptococcal Glomerulonephritis) Tend to Be Volume Expanded and Edematous Due to Sodium Retention (Caused by Increased Sodium Reabsorption in the Collecting Tubules) (Am J Kidney Dis, 2008) [MEDLINE]
- Elevation in blood pressure is primarily due to fluid overload, as evidenced by suppression of the renin-angiotensin-aldosterone system and enhanced release of atrial natriuretic peptide
- Although these changes are most prominent with severe disease, the incidence of hypertension is increased even in patients with a normal serum creatinine concentration
- Both a familial predisposition to hypertension and subclinical volume expansion are thought to be important in this setting
- Patients with Acute Glomerular Disease (Such as Poststreptococcal Glomerulonephritis) Tend to Be Volume Expanded and Edematous Due to Sodium Retention (Caused by Increased Sodium Reabsorption in the Collecting Tubules) (Am J Kidney Dis, 2008) [MEDLINE]
- Clinical
- Acute Kidney Injury (AKI) (see Acute Kidney Injury)
- Hypertension
Autosomal Dominant Polycystic Kidney Disease (ADPCKD) (see Autosomal Dominant Polycystic Kidney Disease)
- Diagnosis
- Abdominal Ultrasound (see Abdominal Ultrasound)
- Clinical
- Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Cysts in Liver, Pancreas, Spleen, and/or Epididymis
- Flank Pain (Due to Renal Hemorrhage (see Flank Pain)
- Hematuria (see Hematuria)
- Hypertension
- Hypertension is Present in the Majority of Patients with Normal Renal Function and Have Reached the 4th Decade of Life
- Hypertension Occurs in Almost 100% of Patients Who Have Advanced End-Stage Renal Disease
- Obstructive Calculi
- Proteinuria (see Proteinuria)
- Urinary Tract Infection (UTI) (see Urinary Tract Infection)
Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Epidemiology
- Hypertension Accounts for Approximately 80-85% of Patients with Chronic Kidney Disease (CKD)
- Chronic Kidney Disease (CKD) is Present in Approximately 14% of Patients with Secondary Hypertension (Circulation, 2025) MEDLINE]
- Diagnosis
- Renal Ultrasound (see Abdominal Ultrasound)
- Useful to Evaluate for Polycystic Kidney Disease, Obstruction, etc
- Serum Chemistry/Complete Metabolic Panel (CMP)
- Abnormal Renal Function (i.e. Elevated Serum Creatinine) Can Be Readily Detected Using a Serum Chemistry Panel
- Urinalysis (see Urinalysis)
- Renal Ultrasound (see Abdominal Ultrasound)
- Clinical
- Fatigue (see Fatigue)
- Frequent Urination
- Peripheral Edema (see Peripheral Edema)
Decreased Nephron Number
- Epidemiology
- Reduced Adult Nephron Mass May Predispose to the Development of Hypertension
- Potential Determinants of Reduced Adult Nephron Mass
- Genetic Factors
- Intrauterine Developmental Disturbance (Such as Hypoxia, Drugs, Nutritional Deficiency)
- Premature Birth
- Postnatal Environment (Including Such Factors as Malnutrition and Infections)
- Potential Determinants of Reduced Adult Nephron Mass
- Reduced Adult Nephron Mass May Predispose to the Development of Hypertension
Renal Artery Stenosis (see Renal Artery Stenosis)
- Epidemiology
- Renal Vascular Disease Accounts for Approximately 0.1-5% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
- Diagnosis
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- In Adults with Hypertension and Atherosclerotic Renal Artery Stenosis, Medical Therapy is Recommended to Reduce Renal and Cardiovascular Disease Morbidity and Mortality (Class of Recommendation: I; Level of Evidence: A)
- In Adults with Hypertension and Atherosclerotic Renal Artery Stenosis for Whom Medical Management Has Failed (Such as Resistant Hypertension, Worsening Renal Function, and/or Acute Heart Failure), it is Reasonable to Refer Patient for Revascularization by Percutaneous Renal Artery Angioplasty and/or Stent Placement (Class of Recommendation: 2a; Level of Evidence: C-EO)
- In Adults with Hypertension and Non-Atherosclerotic Renal Artery Stenosis (Including Fibromuscular Dysplasia), it May Be Reasonable to Refer Patient for Revascularization by Percutaneous Renal Artery Angioplasty (Class of Recommendation: 2b; Level of Evidence: C-LD)
- Renal Ultrasound with Duplex Dopplers (see Renal Ultrasound)
- Renal Magnetic Resonance Angiogram (MRA) (see Renal Magnetic Resonance Angiogram)
- Abdominal/Pelvic Computed Tomography (CT) (see Abdominal/Pelvic Computed Tomography)
- Bilateral Selective Renal Intra-Arterial Angiogram (see Renal Artery Angiogram)
- Recommendations-2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults (Circulation, 2025) MEDLINE]
- Clinical
- Bruit
- Abdominal Systolic-Diastolic Bruit
- Carotid Bruit (Due to Atherosclerotic or Fibromuscular Dysplasia Disease)
- Femoral Bruit
- Clinical Features Suggesting Renal Vascular Disease as an Etiology of Hypertension
- Abrupt Onset/Worsening/Increasingly Difficult to Control Hypertension
- Early-Onset Hypertension (Especially in Females, Associated with Fibromuscular Hyperplasia)
- Flash Pulmonary Edema (Atherosclerotic)
- Resistant Hypertension
- Bruit
Scleroderma (see Scleroderma)
- Epidemiology
- Hypertension is Also Common in Acute Vascular Diseases, Such as Vasculitis or Scleroderma Renal Crisis
- Elevation in blood pressure results from ischemia-induced activation of the renin-angiotensin system rather than volume expansion (Am J Kidney Dis, 2008) [MEDLINE]
- Hypertension is Also Common in Acute Vascular Diseases, Such as Vasculitis or Scleroderma Renal Crisis
- Clinical
- Hypertension
Reproductive
Hemolysis Elevated Liver Functions Low Platelets (HELLP) Syndrome (see xxxx)
- Epidemiology
- Occurs During Pregnancy (see Pregnancy)
- Clinical
- Hemolysis (see Hemolytic Anemia)
- Increased Liver Function Tests (LFT’s) (see Increased Liver Function Tests)
- Jaundice (see Jaundice)
- Hypertension
- Hypertension Occurs in 82-88% of Cases
- Malaise (see Malaise)
- Nausea/Vomiting (see Nausea/Vomiting)
- Proteinuria (see Proteinuria)
- Right Upper Quadrant/Epigastric Pain (see Abdominal Pain)
- Thrombocytopenia (see Thrombocytopenia)
- Visual Changes
Preeclampsia/Eclampsia (see Preeclampsia/Eclampsia)
- Epidemiology
- Occurs During Pregnancy (see Pregnancy)
- Clinical
- Acute Kidney Injury (AKI) (see Acute Kidney Injury)
- Headache (see Headache)
- Increased Liver Function Tests (LFT’s) (see Increased Liver Function Tests)
- Proteinuria (see Proteinuria)
- Pulmonary Edema/Acute Respiratory Distress Syndrome (ARDS) (see Acute Respiratory Distress Syndrome)
- Seizures (see Seizures)
- Occurs in Eclampsia
- Thrombocytopenia (see Thrombocytopenia)
- Visual Changes
Rheumatologic
Vasculitis (see Vasculitis)
- Epidemiology
- Hypertension is also common in acute vascular diseases, such as vasculitis or scleroderma renal crisis
- Elevation in blood pressure results from ischemia-induced activation of the renin-angiotensin system rather than volume expansion (Am J Kidney Dis, 2008) [MEDLINE]
- Hypertension is also common in acute vascular diseases, such as vasculitis or scleroderma renal crisis
Drug/Toxin
General Comments
- Drug or Alcohol-Induced Hypertension Accounts for 2-20% of Secondary Hypertension Cases (Circulation, 2025) MEDLINE]
Acetaminophen (Tylenol) (see Acetaminophen)
- Epidemiology
- When Given at Doses of 4 g/Day for Several Weeks or More
Amphetamine (se Amphetamine)
- Agents
- Amphetamine
- Dexmethylphenidate
- Dextroamphetamine
- Lisdexamphetamine
- Methylphenidate (Ritalin) (see Methylphenidate)
- Pharmacology
- Amphetamine is a Sympathomimetic
- Clinical
- Hypertension
- Tachycardia (see Sinus Tachycardia)
Anti-Androgenic Agents
- Etiology
- Abiraterone (Zytiga) (see Abiraterone)
- Epidemiology
- Single Center, Retrospective, Cohort Study of Patients with Metastatic Prostate Cancer (Ann Pharmacother, 2024) [MEDLINE]
- Patients Who Received Abiraterone Acetate for Metastatic Prostate Cancer Had a Significantly Higher Incidence and Severity of Hypertension (Regardless of Prednisone Dose)
- Pharmacology
- Abiraterone is a CYP17 Inhibitor (Androgen Biosynthesis Inhibitor in Prostate, Testes, and Adrenal Glands)
- Results in Mineralocorticoid Excess with Hypertension, Fluid Retention, and Hypokalemia (see Hypokalemia)
- Epidemiology
- Orteronel
- Androgen Biosynthesis Inhibitor
- Enzalutamide (Xtandi) (see Enzalutamide)
- Pharmacology
- Androgen Receptor Antagonsist
- Pharmacology
- Abiraterone (Zytiga) (see Abiraterone)
Antidepressants
- Agents
- Monoamine Oxidase (MAO) Inhibitors (see Monoamine Oxidase Inhibitors)
- Monoamine Oxidase (MAO) Inhibitors are Particularly Prone to Cause Hypertension (and Potentially a Hypertensive Crisis) with the Consumption of Tyramine-Containing Foods (Aged Cheeses, Cured Meats, Fermented Foods, Draft Beer/Some Wines, Overripe Bananas/Avocados, etc)
- Serotonin–Norepinephrine Reuptake Inhibitors (SNRI’s) (see Serotonin–Norepinephrine Reuptake Inhibitors)
- Tricyclic Antidepressants (TCA’s) (see Tricyclic Antidepressants)
- Monoamine Oxidase (MAO) Inhibitors (see Monoamine Oxidase Inhibitors)
- Management
- Avoid Tyramine-Containing Foods in Conjunction with MAO Inhibitor Use
Atypical Antipsychotics
- Agents
- Clozapine (Clozaril) (see Clozapine)
- Olanzapine (Zyprexa) (see Olanzapine)
- Risperidone (Risperdal) (see Risperidone)
Bevacizumab (Avastin) (see Bevacizumab)
- Epidemiology
- In Patients with Advanced Cancer, Bevacizumab is Associated with 4x Higher Risk for Hypertension
- Intravitreal Bevacizumab Administration is Also Associated with the Hypertension in All Ages (Although Results are Mixed)
- Risk Factors
- Advanced Age
- Dose (Risk May Be Increased with Higher Doses)
- Genetic Polymorphisms of VEGF
- Hyperlipidemia (see Hyperlipidemia)
- Obesity (see Obesity)
- Preexisting Hypertension/Cardiovascular Disease
- Previous Treatment with Anthracycline
- In Patients with Advanced Cancer, Bevacizumab is Associated with 4x Higher Risk for Hypertension
- Pharmacology
- Vascular Endothelial Growth Factor (VEGF)-A Inhibitor
Caffeine (see Caffeine)
- Epidemiology
- Coffee Use in Patients with Hypertension is Associated with Acute Increases in Blood Pressure
- Long-Term Caffeine Use is Not Associated with Increased Blood Pressure or Cardiovascular Disease
- Management
- Generally Limit Caffeine Intake to <300 mg Per Day
- Avoid Use in Patients with Uncontrolled Hypertension
Calcineurin Inhibitors
- Agents
- Cyclosporine A (CSA) (see Cyclosporine)
- Tacrolimus (Prograf) (see Tacrolimus)
- Management
- Tacrolimus is Associated with Fewer Hypertensive Effects than Cyclosporine
Cocaine Intoxication (see Cocaine)
- Pharmacology
- Cocaine is a Sympathomimetic
- Clinical
- Hypertension
- Tachycardia (see Sinus Tachycardia)
Corticosteroids (Systemic) (see Corticosteroids)
- Epidemiology
- Including Both Glucocorticoids and Mineralocorticoids
- Agents
- Dexamethasone (see Dexamethasone)
- Fludrocortisone (see Fludrocortisone)
- Methylprednisolone (see Methylprednisolone)
- Prednisone (see Prednisone)
- Prednisolone (see Prednisolone)
Cyanide Intoxication (see Cyanide)
- Clinical
- Hypertension Occurs Early in the Course of Cyanide Intoxication
Decongestants
- Agents
- Phenylephrine (see Phenylephrine)
- Pseudoephedrine (see Pseudoephedrine)
- Management
- Use for Shortest Duration Possible and Avoid in Severe/Uncontrolled Hypertension
- Consider Alternative Therapies (Such as Nasal Saline, Intranasal Corticosteroids, Antihistamines), as Appropriate
Eculizumab (Soliris) (see Eculizumab)
- Epidemiology
- Hypertension Has Been Reported
- Infants/Children: 22%
- Adolescents/Adults: 17-59%
- Severe Hypertension: 5-9%
- Hypertension Has Been Reported
Erythropoiesis-Stimulating Agents
- Agents
- Erythropoietin (see Erythropoietin)
- Epidemiology
- Erythropoietin-Induced Hypertension Has Been Reported in the Setting of Chronic Kidney Disease (CKD) (Cureus, 2021) [MEDLINE]
- Risk Factors for Erythropoietin-Induced Hypertension
- Family History of Hypertension
- Intravenous Administration (vs Subcutaneous Administration)
- Hemodialysis vs Continuous Ambulatory Peritoneal Dialysis (CAPD) or No Dialysis
- Higher Erythropoiesis-Stimulating Agent Dose
- Higher Hemoglobin Target
- Pharmacology
- Enhanced Vascular Responsiveness to Vasoconstrictors (and Impaired Action of Vasodilators)
- Role of Blood Viscosity is Doubtful
- Enhanced Vascular Responsiveness to Vasoconstrictors (and Impaired Action of Vasodilators)
- Management
- Incidence of Hypertension Can Be Decreased by Achieving Slow Correction of Anemia and by Switching to a Subcutaneous Route of Administration
Ethanol (see Ethanol)
- Epidemiology
- The Direct Relationship Between Alcohol Consumption and Blood Pressure was First Reported in 1915 and Has Been Repeatedly Identified in Contemporary Cross-Sectional and Prospective Cohort Studies
- Alcohol Restriction Decreases Blood Pressure in Patients with Increased Alcohol Intake
- The Direct Relationship Between Alcohol Consumption and Blood Pressure was First Reported in 1915 and Has Been Repeatedly Identified in Contemporary Cross-Sectional and Prospective Cohort Studies
Ethylene Glycol Intoxication (see Ethylene Glycol)
- Clinical
- Mild Hypertension May Be Observed During the Early-Mid Course, While Hypotension Predominates Late in the Course of Ethylene Glycol Intoxication
Glycyrrhizin (Traditional Black Licorice)
- Epidemiology
- Compound Found in Traditional Black Licorice
Herbal Supplements
- Etiology
- Arnica (Plast Reconstr Surg, 2013) [MEDLINE]
- Bitter Orange (Plast Reconstr Surg, 2013) [MEDLINE]
- Blue Cohosh (Plast Reconstr Surg, 2013) [MEDLINE]
- Dong Quai (Plast Reconstr Surg, 2013) [MEDLINE]
- Ginkgo (Plast Reconstr Surg, 2013) [MEDLINE]
- Guarana (Plast Reconstr Surg, 2013) [MEDLINE]
- Ma Huang (Ephedra) (see Ephedra) (Plast Reconstr Surg, 2013) [MEDLINE]
- Pennyroyal Oil (Plast Reconstr Surg, 2013) [MEDLINE]
- Scotch Broom (Plast Reconstr Surg, 2013) [MEDLINE]
- Senna (Plast Reconstr Surg, 2013) [MEDLINE]
- Southern Bayberry (Plast Reconstr Surg, 2013) [MEDLINE]
- St. John’s Wort (in Conjunction with MAO Inhibitors, Yohimbine) (see St John’s Wort) (Plast Reconstr Surg, 2013) [MEDLINE]
- Yohimbine (see Yohimbine) (Plast Reconstr Surg, 2013) [MEDLINE]
Ketamine (Ketalar) (see Ketamine)
- Epidemiology
- Hypertension Occurs Shortly After Intravenous (IV) Ketamine Injection
- Blood Pressure Generally Returns to Normal within 15 min After Ketamine Injection
- Hypertension Occurs Shortly After Intravenous (IV) Ketamine Injection
Kratom (Mitragynia Speciosa Korth) (see Kratom)
- Clinical
- Cardiovascular
- Hypertension (see Hypertension)
- Occurs in 10% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Sinus Tachycardia (see Sinus Tachycardia)
- Occurs in 21% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Hypertension (see Hypertension)
- Neuropsychiatric
- Agitation/Irritability (see Agitation and Irritability)
- Occurs in 23% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Confusion (see Delirium)
- Occurs in 11% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Drowsiness/Lethargy/Coma (see ObtundationComa)
- Seizures (see Seizures)
- Occurs in 10% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Agitation/Irritability (see Agitation and Irritability)
- Other
- Nausea/Vomiting (see Nausea/Vomiting)
- Nausea Occurs in 15% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Vomiting Occurs in 13% of Cases (Clin Toxicol-Phila, 2019) [MEDLINE]
- Cardiovascular
Methylenedioxypyrovalerone (MDPV, Bath Salts) (see Synthetic Cathinones)
- Epidemiology
- Drug of Abuse
- Pharmacology
- Increased Synaptic Concentrations of Dopamine, Serotonin, and/or Norepinephrine Neurotransmitters
- Stimulation of α-Adrenergic and β-Adrenergic Receptors
- Increased Synaptic Concentrations of Dopamine, Serotonin, and/or Norepinephrine Neurotransmitters
- Clinical
- Agitation (see Agitation)
- Diaphoresis (see Diaphoresis)
- Hypertension
- Palpitations (see Palpitations)
- Tachycardia (see Sinus Tachycardia)
Methamphetamine Intoxication (see Methamphetamine)
- Epidemiology
- Drug of Abuse
- Pharmacology
- Methamphetamine is a Sympathomimetic
- Clinical
- Agitation (see Agitation)
- Diaphoresis (see Diaphoresis)
- Hypertension
- Palpitations (see Palpitations)
- Tachycardia (see Sinus Tachycardia)
Metoclopramide (Reglan) (see Metoclopramide)
- Epidemiology
- Cases Have Been Reported (Ann Pharmacother, 2013) [MEDLINE]
Nintedanib (Ofev) (see Nintedanib)
- Epidemiology
- Hypertension Occurs in 5% of Cases
Nonsteroidal Anti-Inflammatory Drug (NSAID’s) (see Nonsteroidal Anti-Inflammatory Drug)
- Pharmacology
- Increased Renal Sodium Reabsorption, Usually Resulting in a Moderate Increase in Blood Pressure
- Management
- Avoid Systemic Nonsteroidal Anti-Inflammatory Drug (NSAID’s) When Possible
- Consider Alternative Analgesics (Such as Acetaminophen, Tramadol, Topical NSAID’s), Depending on Indication and Risk
Oral Contraceptives (OCP’s)
- Epidemiology
- Particularly Oral Contraceptives Containing Higher Doses of Estrogen
- Management
- Use low-dose (eg, 20–30 mcg ethinyl estradiol) agentsS5.4.1-16 or a progestin-only form of contraception, or consider alternative forms of birth control where appropriate (eg, barrier, abstinence, IUD)
- Avoid use in women with uncontrolled hypertension
Serotonin Syndrome (see Serotonin Syndrome)
- Clinical
- Diaphoresis (see Diaphoresis)
- Fever (see Fever)
- Hyperreflexia (see Hyperreflexia)
- Hypertension (More Commonly than Hypotension)
- Myoclonus (see Myoclonus)
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-COV2) (COVID) Vaccination (see Severe Acute Respiratory Syndrome Coronavirus-2 Vaccine)
- Epidemiology
- Post-Vaccination Increased Blood Pressure Has Been Reported (J Cardiovasc Dev Dis, 2022) [MEDLINE]
Tobacco (see Tobacco)
- Epidemiology
- XXXX
Tyrosine Kinase Inhibitors
Withdrawal
Dexmedetomidine Withdrawal (see Dexmedetomidine)
- Epidemiology
- Risk Factors
- Continuous Dexmedetomidine Infusion for a Longer Duration
- Higher Cumulative Daily Dexmedetomidine Dose (>12 mcg/kg/Day)
- Higher Peak Dexmedetomidine Rate (>0.8 mcg/kg/hr)
- History of Hypertension
- Risk Factors
Gabapentin Withdrawal (see Gabapentin)
- Clinical
- Withdrawal Generally Begins Between 12 hrs-7 Days After the Last Dose
- Anxiety/Agitation (see Anxiety and Agitation)
- Depression (see Depression)
- Diaphoresis (see Diaphoresis)
- Dizziness (see Dizziness)
- Headache (see Headache)
- Hypertension
- Insomnia (see Insomnia)
- Muscle Spasm (see Muscle Spasm)
- Nausea/Vomiting (see Nausea/Vomiting)
- Tachycardia (see Tachycardia)
- Tremor (see Tremor)
Rebound Hypertension After Antihypertensive Withdrawal
- Agents
- Clonidine Withdrawal (see Clonidine)
- Clonidine is a Centrally-Acting Sympatholytic (Used to Treat Hypertension)
- β-Blocker Withdrawal (see β-Adrenergic Receptor Antagonists)
- Clonidine Withdrawal (see Clonidine)
Tizanidine Withdrawal (see Tizanidine)
- Pharmacology
- Tizanidine is a Centrally-Acting Sympatholytic (Used to Treat Muscle Spasticity)
Other
Polycythemia Vera (see Polycythemia Vera)
- Epidemiology
- Hypertension Occurs in 46% of Polycythemia Vera Cases (Leukemia, 2013) [MEDLINE]
Ruptured Sinus of Valsalva Aneurysm (see Sinus of Valsalva Aneurysm)
- Epidemiology
- Hypertension May Occur
Physiology
Mechanisms of Hypertension in the Acute Care Setting (Hypertension, 2024) [MEDLINE]
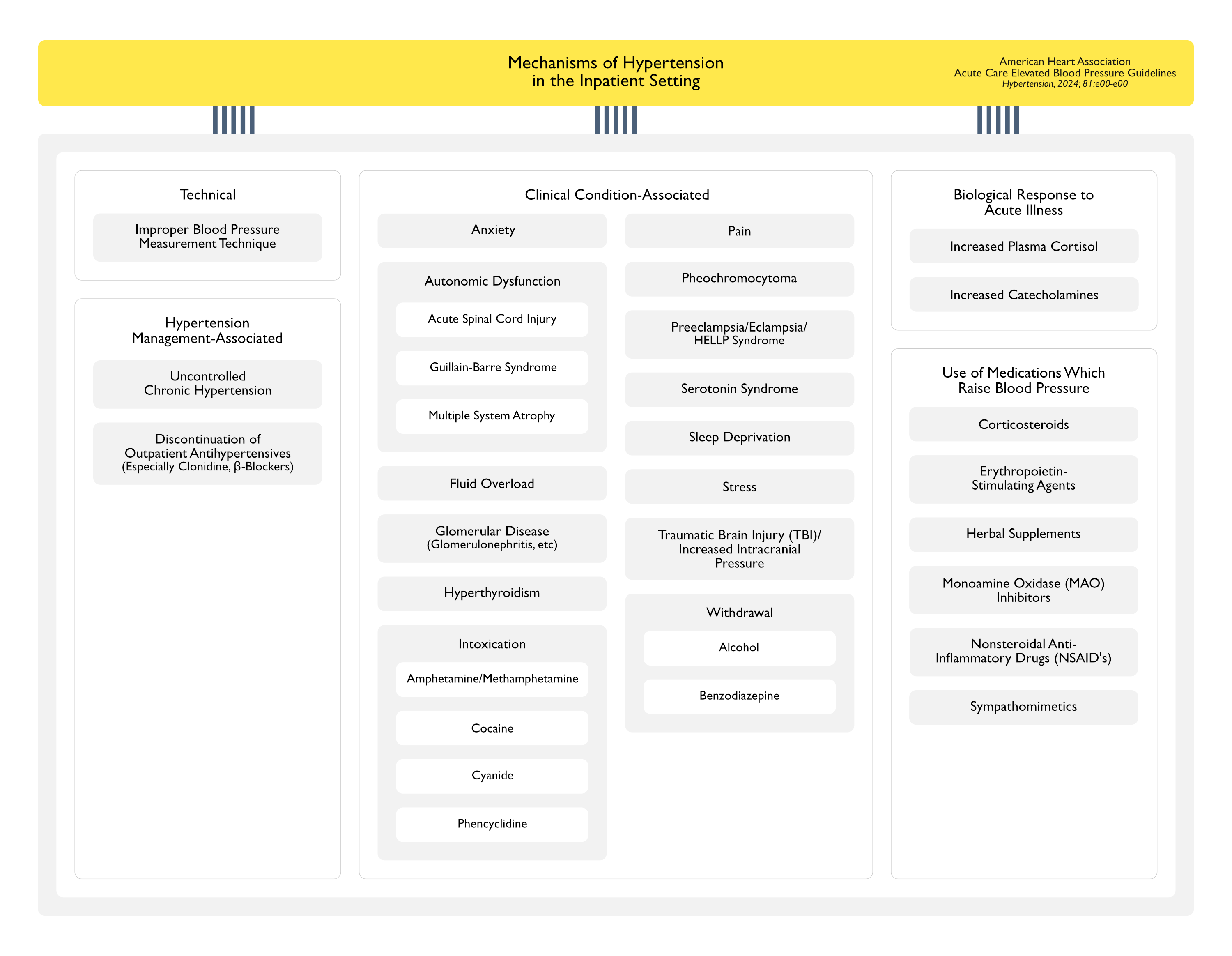
- Uncontrolled Chronic Hypertension
- Biological Responses
- Increased Plasma Cortisol
- Increased Plasma Catecholamines
- Use of Blood Pressure-Raising Medications
- Corticosteroids (see Corticosteroids)
- Erythropoietin-Stimulating Agents (see Erythropoietin)
- Herbal Supplements
- Nonsteroidal Anti-Inflammatory Drugs (NSAID’s) (see Nonsteroidal Anti-Inflammatory Drugs)
- Stimulants
- Cocaine (see Cocaine)
- Methamphetamine (see Methamphetamine)
- Change in Medication Use from Home Environment
- Discontinuation of Outpatient Antihypertensives
- One Study Reported that 41% of Patients Prescribed As-Needed Antihypertensives were Not Receiving Their Outpatient Antihypertensive Regimen During Hospitalization (Ther Adv Cardiovasc Dis, 2018) [MEDLINE]
- Another Study of Postsurgical Inpatients Receiving ≥1 Dose of Intravenous Antihypertensive Medication Found that 25% of Patients were Not Started on Their Outpatient Antihypertensive Medication Regimen During Hospitalization (Am Surg, 2012) [MEDLINE]
- Withdrawal from Substances/Medications
- Discontinuation of Outpatient Antihypertensives
- Inappropriate Blood Pressure Measurement Technique
- Discrepancies Between Blood Pressure Cuff Device Measurements and Arterial Line-Measurements (in Critically Ill Patients)
- Blood Pressure Measured without High-Quality Standards or with a Malfunctioning Device
- Discrepancies in Patient Position/Position Relative to the Heart/Arm Support
- Incorrect Blood Pressure Cuff Size
- Leg Crossing
- Sleep Deprivation/Poor Sleep Hygiene During Hospitalization
- Acute Distress
- Clinical Condition
- Pheochromocytoma (see Pheochromocytoma)
- Thyroid Storm (see Hyperthyroidism)
- Volume Overload
- Acute Kidney Injury (AKI) (see Acute Kidney Injury)
- Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Congestive Heart Failure (CHF) (see Congestive Heart Failure)
References
General
- Prevalence and management of hypertension in the inpatient setting: a systematic review. J Hosp Med.2011;6:417–422. doi: 10.1002/jhm.804 [MEDLINE]
- Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia. 2013;27(9):1874 [MEDLINE]
- Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013 Mar;44(3):870-947. doi: 10.1161/STR.0b013e318284056a [MEDLINE]
- A New Guideline on Treatment of Hypertension in Those with Coronary Artery Disease: Scientific Statement From the American Heart Association, American College of Cardiology, and American Society of Hypertension About Treatment of Hypertension in Patients with Coronary Artery Disease. Heart Lung Circ. 2015 Nov;24(11):1037-40. doi: 10.1016/j.hlc.2015.05.022 [MEDLINE]
- 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018 Jun;71(6):e13-e115. doi: 10.1161/HYP.0000000000000065 [MEDLINE]
- Definitions and Epidemiological Aspects of Hypertensive Urgencies and Emergencies. High Blood Press Cardiovasc Prev. 2018 Sep;25(3):241-244. doi: 10.1007/s40292-018-0263-2 [MEDLINE]
- 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018 Mar;49(3):e46-e110. doi: 10.1161/STR.0000000000000158 [MEDLINE]
- Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. Stroke. 2019 Dec;50(12):3331-3332. doi: 10.1161/STROKEAHA.119.027708 [MEDLINE]
- Hypertensive emergencies and urgencies in emergency departments: a systematic review and meta-analysis. J Hypertens. 2020 Jul;38(7):1203-1210. doi: 10.1097/HJH.0000000000002372 [MEDLINE]
- Primary Care of Adult Patients After Stroke: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke. 2021 Aug;52(9):e558-e571. doi: 10.1161/STR.0000000000000382 [MEDLINE]
- Treatment and outcomes of inpatient hypertension among adults with noncardiac admissions. JAMA Intern Med. 2021;181:345–352. doi:
- Severe inpatient hypertension prevalence and blood pressure response to antihypertensive treatment. J Clin Hypertens (Greenwich). 2022;24:339–349. doi: 10.1111/jch.14431 [MEDLINE]
- 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-e361. doi: 10.1161/STR.0000000000000407 [MEDLINE]
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-e1032. doi: 10.1161/CIR.0000000000001063 [MEDLINE]
Etiology
- Independent effects of weight change and attained body weight on prevalence of arterial hypertension in obese and non-obese men. BMJ. 1989;299(6702):767 [MEDLINE]
- Essential hypertension. Lancet. 2003;361(9369):1629 [MEDLINE]
- Blood pressure change and risk of hypertension associated with parental hypertension: the Johns Hopkins Precursors Study. Arch Intern Med. 2008;168(6):643 [MEDLINE]
- Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302(4):401 [MEDLINE]
- Sustained hypotension following intravenous metoclopramide. Ann Pharmacother. 2013;47(11):1577-1580. doi:10.1177/1060028013503789 [MEDLINE]
- Herbal products that may contribute to hypertension. Plast Reconstr Surg. 2013 Jan;131(1):168-173. doi: 10.1097/PRS.0b013e318272f1bb [MEDLINE]
- Erythropoietin-Induced Hypertension: A Review of Pathogenesis, Treatment, and Role of Blood Viscosity. Cureus. 2021 Jan 20;13(1):e12804. doi: 10.7759/cureus.12804 [MEDLINE]
- Blood Pressure Increase following COVID-19 Vaccination: A Systematic Overview and Meta-Analysis. J Cardiovasc Dev Dis. 2022 May 9;9(5):150. doi: 10.3390/jcdd9050150 [MEDLINE]
- Real-World Incidence and Severity of Hypertension Caused by Abiraterone Acetate in Patients With Metastatic Prostate Cancer. Ann Pharmacother. 2024 Feb 12:10600280231223213. doi: 10.1177/10600280231223213 [MEDLINE]
Physiology
- As-needed antihypertensive therapy in surgical patients, why and how: challenging a paradigm. Am Surg. 2012;78:250–253 [MEDLINE]
- Retrospective review of the use of as-needed hydralazine and labetalol for the treatment of acute hypertension in hospitalized medicine patients. Ther Adv Cardiovasc Dis. 2018;12:7–15. doi: 10.1177/1753944717746613 [MEDLINE]