Diffuse Panbronchiolitis
Epidemiology
- Seen mainly in Asia (mostly in Japan), few case reports in North America and Europe
- Not associated with smoking
- Usually occurs in males >40 y/o
- Associated With
- Adult T-cell leukemia
- Ulcerative Colitis
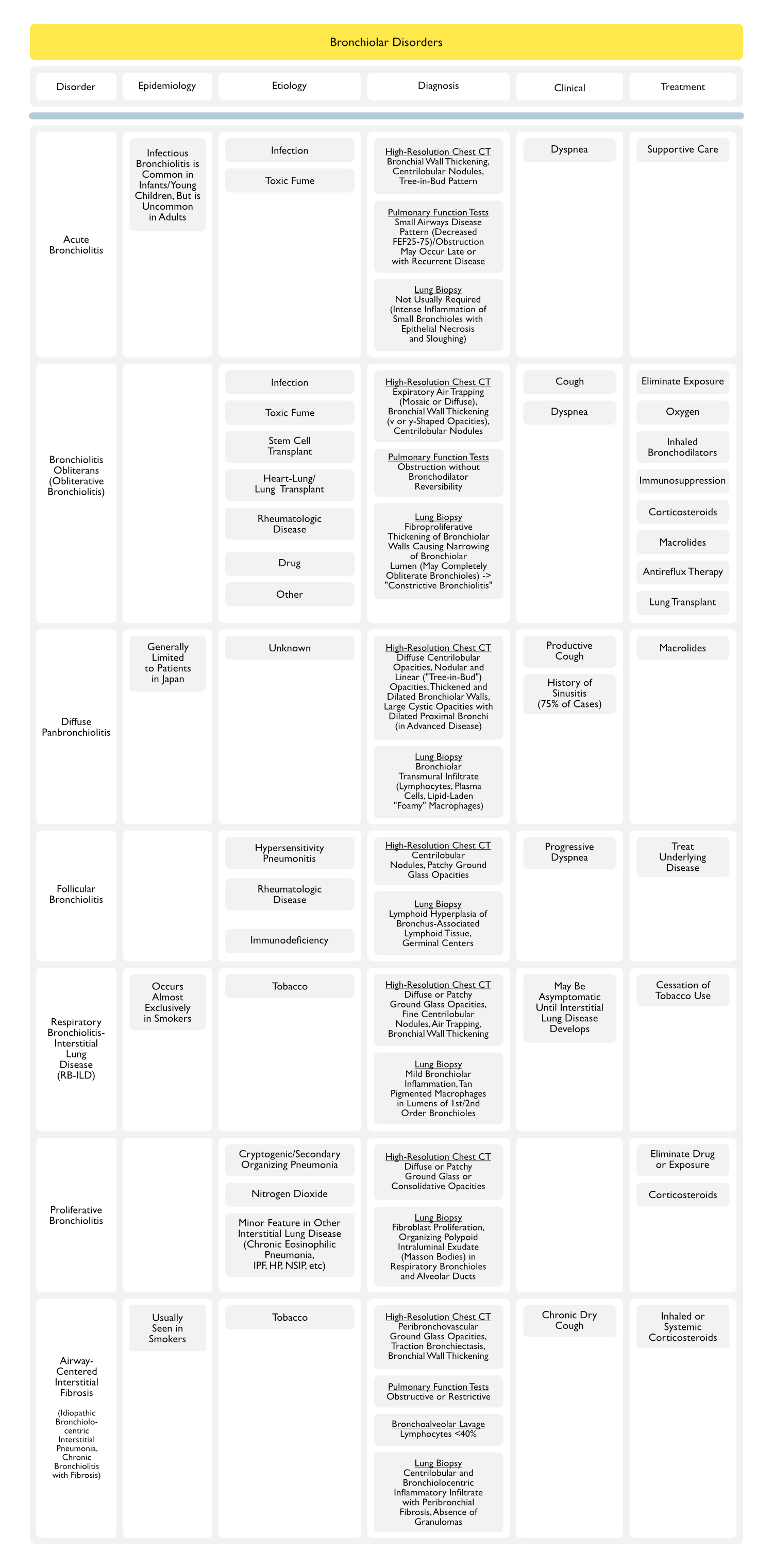
Etiology
Physiology
- Unclear
- Normal ciliary function
- Pseudomonas infection occurs late in disease course
Pathologic Pattern
- Obliterative or proliferative BO may be seen
- Peribronchiolar mononuclear infiltrate involving entire wall of respiratory bronchiole (lumen filled with acute inflammatory cells: neutrophils)
- Intraalveolar foamy macrophages: within peribronchiolar alveolar septa
- Proximal bronchiectasis:
Diagnosis
- PFT’s: obstructive pattern
- FOB: BAL reveals moderately increased WBC with neutrophilic predominance
- Intraluminal acute inflammatory exudate usually represent superimposed bacterial infection
- CXR/Chest CT Patterns
- Interstitial small nodular infiltrates (lower zone predominance) with hyperinflation:
- HRCT: panbronciolitis/ bronchiectasis/ small linear branching opacities/ small nodules in centrilobular areas
- Ig levels: normal
Clinical
- Rapidly Progressive Airway Obstruction (see [[Obstructive Lung Disease]])
- Chronic Sinusitis: typical
Treatment
- Low-Dose Erythromycin
- Dose: 200 mg PO qday
- Marked improvement in symptoms and CXR (unclear mechanism)
- Steroids/Immunosuppressives: no role in this disease
References