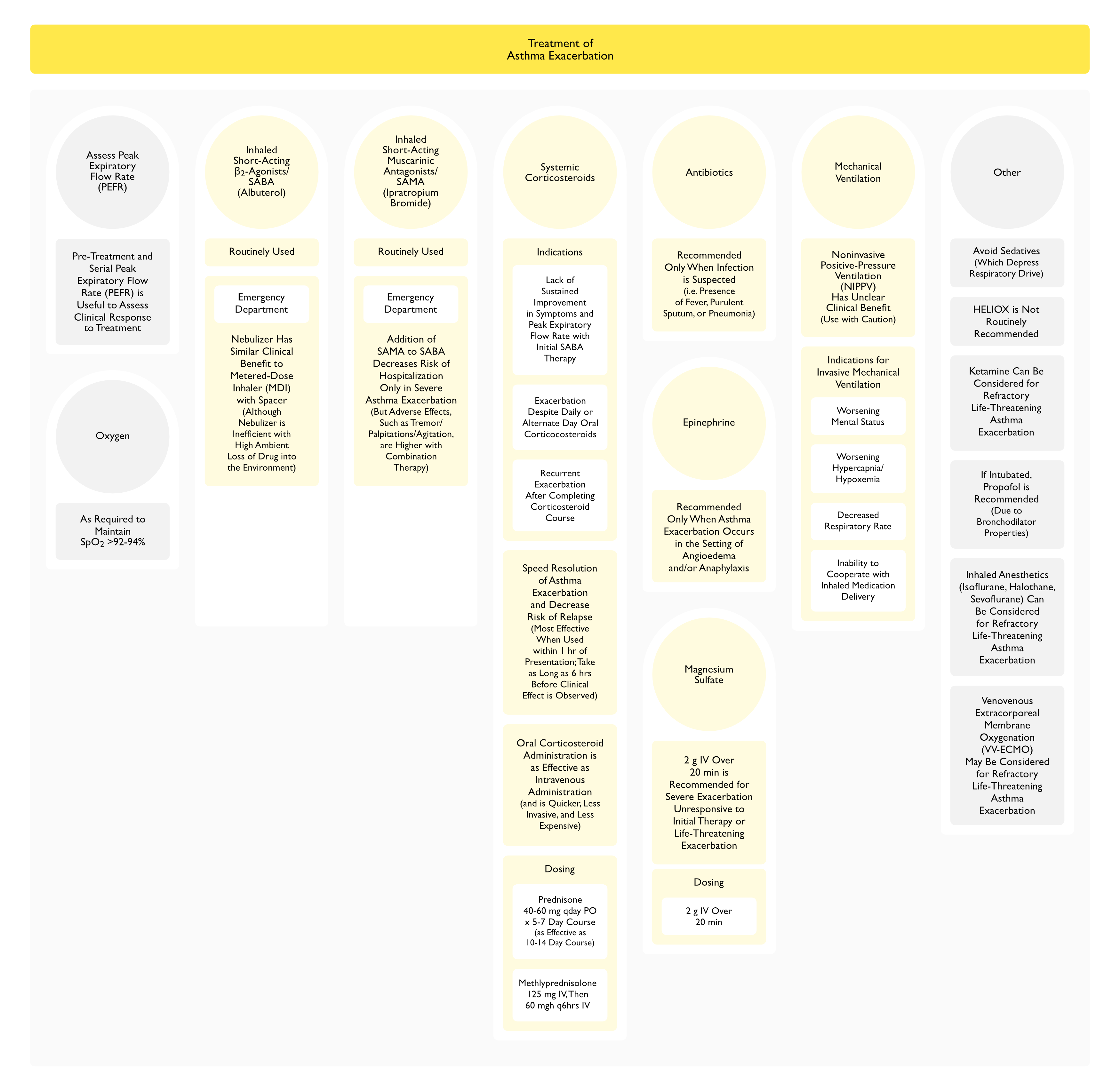
Treatment-Asthma Exacerbation
General Comments
- Avoid Histaminergic Agents
- Avoid Morphine (see Morphine)
- xxxx
Prediction of Need for Hospital Admission for Asthma Exacerbation
- xxxx
[LINK]

Antibiotics
Clinical Efficacy
- Trial of Telithromycin in Acute Asthma Exacerbation (NEJM, 2006) [MEDLINE] (see Telithromycin)
- Telithromycin Decreased Asthma Symptoms, But Had No Other Clinical Efficacy
- Approximately 61% of Patients had Elevated Antibody Titers for Mycoplasma Pneumoniae or Chlamydophila Pneumoniae: however, bacteriologic status was not associated with clinical response to treatment
- Trial Examining the Efficacy of Procalcitonin Use to Guide Antibiotic Therapy in Acute Asthma Exacerbation (BMC Infect Dis, 2013) [MEDLINE] (see Serum Procalcitonin)
- Serum Procalcitonin Can Be Used to Guide the Use of Antibiotic Therapy in Acute Asthma Exacerbation
- UK Double-Blind, Placebo-Controlled, Randomized Trial of Azithromycin (x 3 Days) in Adults with Acute Asthma Exacerbation (JAMA Intern Med, 2016) [MEDLINE] (see Azithromycin)
- Azithromycin Treatment Had No Clinical Benefit
- In the Trial, 5% of Azithromycin-Treated Patients were Positive for Mycoplasma Pneumoniae or Chlamydophila Pneumoniae
- For Each 10 Patients Randomized, >10 Patients were Excluded (Approximately 45% of the Total Screened Patient Population) Because They Already Had Received Antibiotics: this may have resulted in selection bias
General Recommendations
- Antibiotics are Probably Only Useful to Treat Concomitant Bacterial Infections (Such as Pneumonia, Sinusitis, etc) in the Setting of Acute Asthma Exacerbation: since most respiratory infections which trigger acute asthma exacerbation are viral, rather than bacterial
Recommendations (Global Initiative for Asthma/GINA Guidelines 2016) [MEDLINE]
- Antibiotics are Not Recommended in the Management of Acute Asthma Exacerbation
Epinephrine (see Epinephrine)
Clinical Efficacy
- xx
Recommendations
- Epinephrine is Recommended Only in Asthma Exacerbations Associated with Angioedema or Anaphylaxis (see Angioedema and )
Magnesium Sulfate (see Magnesium Sulfate)
Pharmacology
- Magnesium Has Bronchodilator Properties, Possibly Due to Inhibition of Calcium Influx into Airway Smooth Muscle Cells
Contraindications
- Renal Failure
- Acute Kidney Injury (AKI) (see Acute Kidney Injury)
- Chronic Kidney Disease (CKD) (see Chronic Kidney Disease)
- Hypermagnesemia (see Hypermagnesemia)
Clinical Efficacy
- Small Early Trial of Intravenous Magnesium Sulfate for Acute Asthma Exacerbation in the Emergency Department (JAMA, 1989) [MEDLINE]
- Intravenous Magnesium Sulfate Improved PEFR and Decreased Hospital Admissions
- MAGNETIC Trial of Nebulized Isotonic Magnesium Sulfate in Children with Acute Asthma Exacerbation (Lancet Resp Med, 2013) [MEDLINE]
- Nebulized Isotonic Magnesium Sulfate Did Not Impact Asthma Severity Score in Children with Acute Asthma Exacerbation
- However, the Greatest Benefit was Observed in Children with More Severe Asthma Exacerbations (SaO2 <92% at Presentation and with Preceding Symptoms Lasting <6 hrs)
- Small Trial of Nebulized Magnesium in Adults with Acute Asthma Exacerbation in the Emergency Department (Pulm Pharmacol Ther, 2010) [MEDLINE]: n = 30, FEV1 <60% predicted
- Adding Nebulized Magnesium Sulfate to Standard Therapy in Severe Asthma Exacerbation Improved FEV1 and Oxygen Saturation and Decreased the Rate of Hospital Admission
- Systematic Review of Nebulized Magnesium Sulfate in Acute Asthma Exacerbation (Cochrane Database Syst Rev, 2012) [MEDLINE]
- Overall, Add-On Nebulized Magnesium Sulfate Did Not Improve Pulmonary Function or Decrease Hospital Admissions
- Individual Results from Three Trials Suggest that Nebulized Magnesium Sulfate Might Improve Pulmonary Function in a Subset of Patients with Severe Asthma Exacerbations (FEV1 <50% Predicted)
- Overall, Add-On Nebulized Magnesium Sulfate Did Not Improve Pulmonary Function or Decrease Hospital Admissions
- UK Double-Blind, Randomized, Controlled 3Mg Trial of Intravenous or Nebulized Magnesium Sulfate in Adults with Acute Asthma Exacerbation (Lancet Respir Med, 2013) [MEDLINE]: patients ≥16 y/o
- Patients with Life-Threatening Features were Excluded from the Study
- Neither Nebulized or Intravenous Magnesium Sulfate Decreased the Rate of Hospital Admission or Dyspnea, as Compared to Placebo
- Systematic Review of Intravenous Magnesium Sulfate in Adults with Acute Asthma Exacerbation in the Emergency Department (Cochrane Database Syst Rev, 2014) [MEDLINE]
- Single Infusion of Intravenous Magnesium Sulfate (1.2-2g Over 15-30 min) Decreased Hospital Admissions and Improved Lung Function in Patients Who Have Not Responded to Oxygen, Nebulized β2 Agonists, and Intravenous Corticosteroids
- However, Differences in the Ways the Trials were Conducted Made it Difficult for the Authors to Assess Whether Severity of the Exacerbation or Additional Co-Medications Altered the Treatment Effect of Magnesium Sulfate
- Systematic Review of Nebulized Magnesium Sulfate in Acute Asthma Exacerbation (Cochrane Database Syst Rev, 2017) [MEDLINE]
- Nebulized Magnesium Sulfate Add-On Therapy (to Nebuilzed β2-Agonists and Ipratropium Bromide) May Have Modest Benefits in Terms of Lung Function and Hospital Admissions: however, confidence in this evidence is low
- Individual Studies Suggest that Those with More Severe Asthma Exacerbations and Exacerbations of Shorter Duration May Experience a Greater Clinical Benefit: however, further research into subgroups is warranted
- Nebulized Magnesium Sulfate Does Not Appear to Be Associated with an Increase in Serious Adverse Events
- Nebulized Magnesium Sulfate Add-On Therapy (to Nebuilzed β2-Agonists and Ipratropium Bromide) May Have Modest Benefits in Terms of Lung Function and Hospital Admissions: however, confidence in this evidence is low
Recommendations (National Asthma Education and Prevention Program/NAEPP Guidelines 2007) [MEDLINE]
- Intravenous Magnesium Sulfate (2g Over 20 min) is Suggested for Patients with Life-Threatening Asthma Exacerbation with Persistent Severity (PEFR <40% of Baseline) After 1 hr of Therapy
Recommendations (Global Initiative for Asthma/GINA Guidelines 2016) [MEDLINE]
- Intravenous Magnesium Sulfate is Not Routinely Recommended in Treatment of Acute Asthma Exacerbation
- However, Intravenous Magnesium Sulfate May Decrease Hospital Admission in Select Subsets of Patients (Evidence Level: A)
- Adults with FEV1 <25-30% Predicted at Presentation
- Adults and Children Who Fail to Respond to Initial Treatment and Have Persistent Hypoxemia
- Children Whose FEV1 Fails to Reach 60% Predicted After 1 hr of Care
- However, Intravenous Magnesium Sulfate May Decrease Hospital Admission in Select Subsets of Patients (Evidence Level: A)
Oxygen (see Oxygen)
- xxx
Short-Acting β2-Adrenergic Receptor Agonists (SABA) (see β2-Adrenergic Receptor Agonists)
- xxx
Short-Acting Anti-Muscarinic/Anti-Cholinergic Agents (SAMA) (see Muscarinic Antagonists)
- xxx
Inhaled Corticosteroids
- xxxx
- Adherence to inhaled corticosteroid medications after an asthma exacerbation and the risk of subsequent exacerbations. Ann Allergy Asthma Immunol. 2025 Aug 13:S1081-1206(25)00416-8. doi: 10.1016/j.anai.2025.08.007 [MEDLINE]
- Background: Data on the duration of improved adherence to controller medications after an exacerbation and its impact on asthma outcomes are inconsistent
- Objective: To describe levels and changes in adherence to inhaled corticosteroid (ICS)-containing medication after a severe exacerbation and the association with future exacerbation risk
- Methods: This retrospective cohort study used data from Optum’s deidentified Clinformatics Data Mart Database (October 2015-December 2023). Patients with asthma, 1 or more severe exacerbations, and adherence to ICS-containing therapy (proportion of days covered [PDC]) of less than 80% in the 3 months before an exacerbation were included. Primary and secondary end points were the annualized asthma exacerbation rate and the time to the first subsequent severe exacerbation. End points were compared between patients who improved adherence in the 3 months after the qualifying exacerbation to 80% or more and those who remained at PDC less than 80%. Inverse probability of treatment weighting accounted for between-group imbalances
- Results: Of 68,398 participants, 85% stayed less than 80% PDC, whereas 15% improved to PDC 80% or more at 3 months after the qualifying exacerbation. Of patients with improved PDC, only 40%, 31%, and 22% maintained PDC 80% or more at 3 to 6, 6 to 9, and 9 to 12 months after the qualifying exacerbation, respectively. Improving adherence to PDC 80% or more in the 3 months after the qualifying exacerbation did not reduce annualized asthma exacerbation rate (rate ratio: 0.958 [95% CI 0.912-1.007]) or increase the time to the next exacerbation (hazard ratio: 0.997 [95% CI 0.954-1.041]). Results were consistent in sensitivity analyses
- Conclusion: Improvement in adherence to ICS-containing therapy after a severe exacerbation was transient and not beneficial for exacerbation outcomes, indicating a need to consider alternative treatment strategies in patients with asthma
Systemic Corticosteroids (see Corticosteroids)
Clinical Efficacy
- xxxx
Leukotriene Receptor Antagonists
Agents
- xxxxxx
Clinical Efficacy
- xxxx
Enoximone (see Enoximone)
Clinical Efficacy
- xxxx
Ketamine (see Ketamine)
Pharmacology
- Ketamine is a Dissociative Anesthetic with Bronchodilator Properties
Clinical Efficacy
- xxx
Inhalational Anesthestics
Pharmacology
- Direct Relaxant Effect on Airway Smooth Muscle and Attenuation of Cholinergic Tone Have Both Been Proposed as Mechanism of Action
Agents
- Halothane (see Halothane): greatest amount of clinical data with this agent
- Isoflurane (see Isoflurane)
- Sevoflurane (see Sevoflurane)
Clinical Efficacy
- xxx
Heliox (see Heliox)
Clinical Efficacy
- xxxx
Noninvasive Positive Pressure Ventilation (NIPPV) (see Noninvasive Positive-Pressure Ventilation)
Clinical Efficacy
- Study of NIPPV in Respiratory Failure Due to Asthma Exacerbation (Respirology, 2010) [MEDLINE]
- NIPPV Use in Asthma is Not Well-Defined, But Can Be Considered in Select Patients
- Systematic Review of NIPPV in Asthma Exacerbation (Cochrane Database Syst Rev, 2012) [MEDLINE]
- Use of NIPPV in Asthma Exacerbation Has Unclear Clinical Benefit
- Trial of Nebulization with Noninvasive Ventilation in the Treatment of Asthma Exacerbation (Respiratory Care, 2013) [MEDLINE]
- Coupling Nebulization and NIPPV During the Treatment of Asthma Exacerbation Did Not Improve Pulmonary Radio-Aerosol Deposition, But There was Clinical Improvement of Pulmonary Function
Recommendations
- Role of NIPPV in Asthma Exacerbation is Not Well-Defined
Invasive Mechanical Ventilation (see Mechanical Ventilation-General)
Physiology
- The Endotracheal Tube Itself Adds Another Resistance in Series with the Obstructed Asthmatic Airways
Technique
- Monitoring
- Monitor the PIP – Plateau Pressure Difference (Airway Resistive Pressure)
- PIP- Plateau Pressure Difference Correlates with the Degree of Airway Resistance (Due to Bronchospasm)
- Monitor the PIP – Plateau Pressure Difference (Airway Resistive Pressure)
- Measures to Optimize Pulmonary Mechanics (Maintain Plateau Pressure <30 cm H2O, etc) During Mechanical Ventilation in Asthma
- Sedation (see Sedation): required
- Propofol (Diprivan) (see Propofol): also has bronchodilator properties
- Ketamine (see Ketamine): also has bronchodilator properties (likely due to vagolytic effects)
- General/Inhalational Anesthesia (see General Anesthesia): usually a last resort
- Paralysis (see Neuromuscular Junction Antagonists): use judiciously to avoid complication of prolonged paralysis/myopathy
- Use of Permissive Hypercapnia (J Intensive Care Med, 2018) [MEDLINE]
- Hypercapnia is Common During Mechanical Ventilation in Severe Asthma
- The Term “permissive” is a Misnomer in Many Cases, Since Hypercapnia Occurs Due to Increased Dead Space Ventilation (Due to Alveolar Overdistention) and Attempts to Increase the Minute Ventilation May Cause Further Hyperinflation, Worsening the Physiologic Dead Space (For This Reason, Hypercapnia May Be Inevitable, Rather Than “Permitted”)
- Sodium Bicarbonate May Be Required to Maintain an Adequate pH >7.20
- Use Low Tidal Volumes
- Use Low Respiratory Rate
- Increase Inspiratory Flow Rate: to shorten the inspiratory time and prolong the expiratory time
- Heliox (see Heliox)
- Small Prospective Trial of Heliox in Mechanically Ventilated COPD Patients (Crit Care Med, 2000 [MEDLINE]: n = 23
- In Mechanically-Ventilated COPD Patients with Auto-PEEP (5+/-2.7 cm H2O vs 9+/-2.5 cm H2O), Heliox Decreased Trapped Lung Volume, Auto-PEEP, Peak Inspiratory Pressure (25+/-6 cm H2O vs 30+/-5 cm H2O), and Mean Airway Pressure, as Compared to Usual Care
- In Mechanically-Ventilated COPD Patients with Auto-PEEP, Heliox Did Not Impact Hemodynamics or Arterial Blood Gases
- Small Prospective Trial of Heliox in Mechanically Ventilated COPD Patients (Crit Care Med, 2000 [MEDLINE]: n = 23
- Sedation (see Sedation): required
Complications of Mechanical Ventilation in the Setting of Asthma
- Barotrauma
- Pneumomediastinum (see Pneumomediastinum)
- Pneumopericardium (see Pneumopericardium)
- Pneumothorax (see Pneumothorax)
- Subcutaneous Emphysema (see Subcutaneous Emphysema)
- Development of Auto-PEEP (see PEEP and Auto-PEEP)
- Pulseless Electrical Activity (PEA) (see Pulseless Electrical Activity)
- Physiology
- Due to increased intrathoracic pressure with decreased venous return to the right side of the heart
- Physiology
- Death
American Heart Association (AHA) Recommendations for Adult Basic and Advanced Life Support (2020) (Circulation, 2020) [MEDLINE]
- For Asthmatic Patients with Cardiac Arrest, Sudden Increase in Peak Inspiratory Pressures (PIP) or Difficulty ventilating Should Prompt Evaluation for Tension Pneumothorax (Class of Recommendation: 1, Level of Evidence: C-LD)
- Due to the Potential Effects of Intrinsic Positive End-Expiratory Pressure (Auto-PEEP) and Risk of Barotrauma in an Asthmatic Patient with Cardiac Arrest, a Ventilation Strategy of Low Respiratory Rate and Low Tidal Volume is Reasonable (Class of Recommendation: 2a, Level of Evidence: C-LD)
- If Increased Auto-PEEP or Sudden Decrease in Blood Pressure is Noted in Asthmatics Receiving Bag-Valve-Mask (BVM) Ventilation/Mechanical Ventilation in a Periarrest State, a Brief Disconnection from the Bag-Valve-Mask (BVM) or Ventilator with Compression of the Chest Wall to Relieve Air Trapping Can Be Effective (Class of Recommendation: 2a, Level of Evidence: C-LD)
Venovenous Extracorporeal Membrane Oxygenation (VV-ECMO) (see Venovenous Extracorporeal Membrane Oxygenation)
Clinical Efficacy
- XXXXXX
Agents/Treatments With Unclear or No Clinical Benefit in the Treatment of Asthma Exacerbation
- Aminophylline (see Aminophylline)
- XXXXXXXX
- Furosemide (Lasix) (see Furosemide)
- Clinical Efficacy
- XXXX
- Clinical Efficacy
- Theophylline (Theodur) (see Theophylline)
- Clinical Efficacy
- XXXXX
- Clinical Efficacy
Prognosis of Severe Asthma Exacerbation
- xxxx
- Predicting 30-day in-hospital mortality in ICU asthma patients: a retrospective machine learning study with external validation. BMC Pulm Med. 2025 Aug 12;25(1):387. doi: 10.1186/s12890-025-03881-w [MEDLINE]
- Background: Asthma-related mortality in the intensive care unit (ICU) remains poorly characterized, with no existing predictive models specifically designed for this high-risk population. This study aimed to develop and externally validate a machine learning-based model to predict 30-day in-hospital mortality among ICU patients with asthma
- Methods: The model was developed using data from MIMIC-IV 2.2 and externally validated on a subset of MIMIC-IV 3.1. Clinical variables from the first 24 h of ICU admission were extracted. Feature selection was conducted using both LASSO regression and the Boruta algorithm. Seven machine learning algorithms were trained and evaluated using receiver operating characteristic (ROC) curves, calibration plots, and decision curve analysis. The best-performing model was identified based on internal and external validation results. SHapley Additive exPlanations (SHAP) were employed to interpret feature importance. The final model was deployed as an interactive web-based tool
- Results: A total of 4385 ICU asthma patients were analyzed. The final XGBoost model, using 12 features, achieved the highest AUROC in both internal (0.83) and external (0.80) validation, and demonstrated the best calibration and net clinical benefit. SHAP analysis identified age, respiratory rate, RDW, urine output, and anion gap as top predictors. The model outperformed conventional ICU scores and is available as a web-based tool
- Conclusions: We developed and externally validated a robust prediction model for 30-day mortality in ICU patients with asthma. The model offers strong performance, interpretability, and clinical utility, supporting its use for real-time risk stratification and decision-making in critical care settings.
Pregnancy
- Asthma Remission Rates:
- Childhood Asthma: mild persistent disease may remit but mod-severe disease probably will continue into adulthood (about 50% achieve remission)
- Adult Asthma: middle-aged and older adult asthmatics rarely achieve complete remission (only 10-15% achieve remission, as is defined by being asyptomatic with normal FEV1 and normal airway responsiveness)
- Remission is associated with milder asthma, male gender, younger age at first diagnsosis, and less initial airway responsiveness
- There is a more rapid rate of annual FEV1 decline in asthmatics than there is in normals (this is compunded by smoking)
Mortality Rates: lower mortality rate in USA compared to other countries (possibly due to different patterns of aerosol bronchodilator use)
- Relatively stable mortality rate in USA in 5-34 y/o group since 1960 (but 25% increase in total number of deaths)
- Countries with highest mortality rates usually have highest prevalence
Risk of Fatal Asthma: greatest in those asthmatics with highest degree of airway hyperresponsiveness and FEV1 lability (rather than in those with severe, fixed airway obstruction)
- In patients with >50% FEV1 response to bronchodilator (as compared to those with <25% bronchodilator response): 7-fold higher risk of death from asthma
- Persistent FEV1 lability is most common in smokers and those with persistent atopic asthma
- Other risk factors for asthma mortality: age >40, smoking, and blood eosinophilia
Prognosis
Prognosis of Asthma-COPD Overlap (see xxxx)
- xxxx
- Hospitalization Outcomes of Patients with Asthma, COPD, and Asthma-COPD Overlap Syndrome. Chronic Obstr Pulm Dis. 2025 Jul 30;12(4):260-273. doi: 10.15326/jcopdf.2024.0566 [MEDLINE]
- Background and objectives: Chronic obstructive pulmonary disease (COPD) and asthma account for a significant health care burden within the United States. The asthma-COPD overlap (ACO) phenotype has been associated with increased exacerbation frequency and health care utilization compared to either disease alone. However, hospital-based outcomes of these diagnoses have not been described in the literature
- Methods: Hospitalization data were extracted from the Healthcare Cost and Utilization Project Nationwide Readmissions Database (HCUP-NRD 2012-2015). Using International Classification of Diseases, Ninth Revision, Clinical Modification codes, we classified patients as having asthma, COPD, or ACO. We used analytic sample weights to compute national estimates, and weighted regression analyses to evaluate hospitalization outcomes
- Results: Of 2,522,013 patients reviewed, 1,732,946 (68.7%) had COPD, 668,867 (26.5%) had asthma, and 120,200 (4.8%) had ACO. Patients with ACO were younger than those with COPD (63 versus 69 years old, p< 0.05), with a higher rate of respiratory failure and an increased hospital length of stay. Index admission mortality was higher in patients with COPD (adjusted odds ratios [OR] [95%]: 2.10 [1.84; 2.40]) and asthma (adjusted OR [95%]: 1.59 [1.38; 1.83]) as compared to those with ACO. However, the all-cause readmission rate was higher in the COPD group (15.7%) but not in the asthma group (10.7%) as compared to the ACO group (11.5%)
- Conclusion: While ACO was associated with higher rates of baseline comorbidities, increased length of stay, and higher health care cost during index admission, this did not translate into higher in-hospital mortality, complication rates, or risk for asthma-related readmission mortality when compared to asthma or COPD alone, highlighting the complexity of the ACO disease burden
