Clinical Manifestations
General Comments
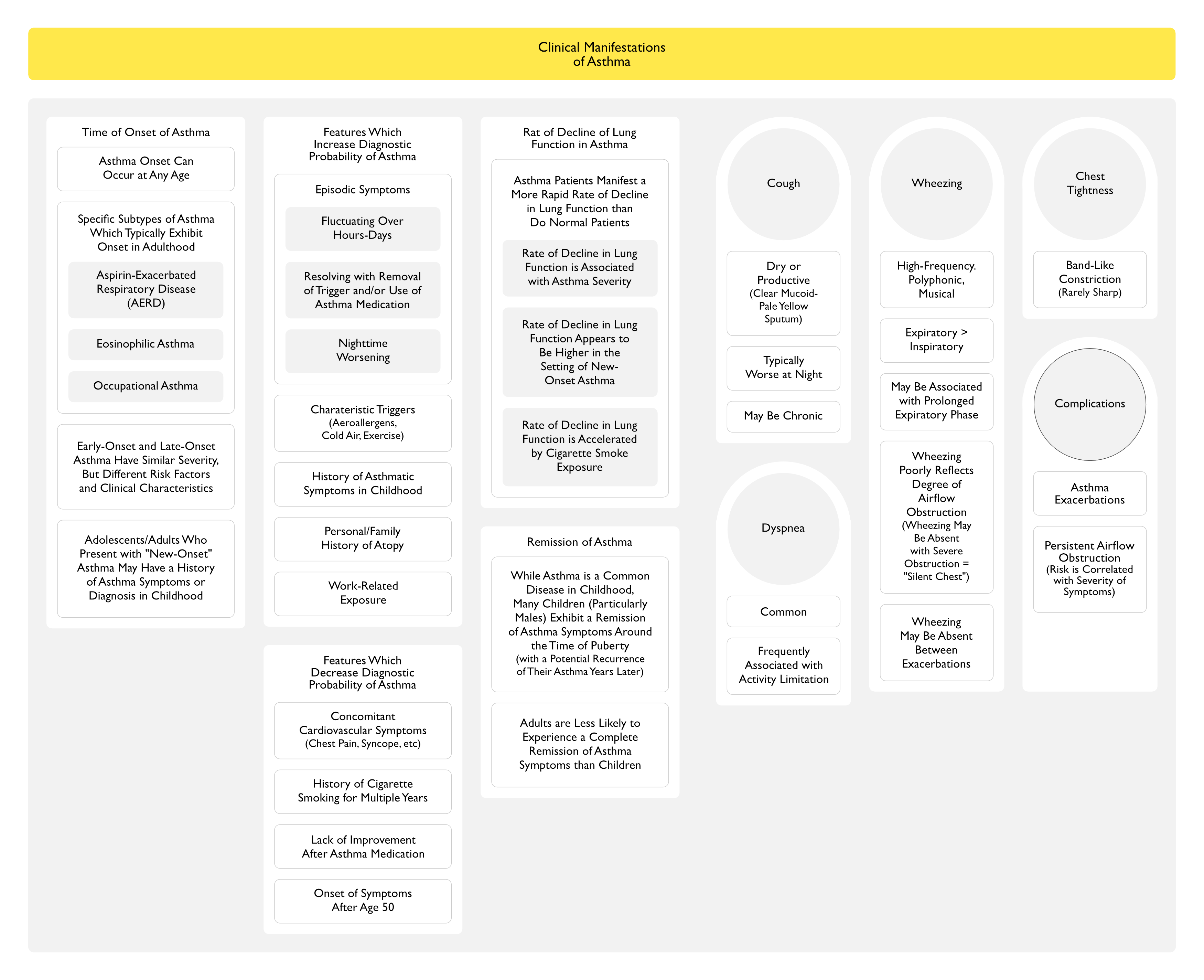
Time of Onset
- Asthma Can Develop at Any Age
- Early-Onset vs Late-Onset Asthma
- Adolescents/Adults Who Present with “New-Onset” Asthma Symptoms May Have a History of Asthma Symptoms or Diagnosis in Childhood (NEJM, 2003) [MEDLINE]
- This is Especially True for Asthma with Onset in Early Adulthood (Lancet, 2008) [MEDLINE]
- Some Studies Suggest that Asthma is Late-Onset in Approximately 50% of Adults with Asthma, with Differing Clinical Characteristics and Risk Factors from Early-Onset Asthma (Ann Am Thorac Soc, 2013) [MEDLINE] (Thorax, 2016) [MEDLINE]
- However, There Appears to Be No Difference in Severity Between Early-Onset and Late-Onset Asthma (Expert Rev Respir Med, 2015) [MEDLINE]
- Cross-Sectional Study of Clinical Features in Adult Asthmatics (J Allergy Clin Immunol Pract, 2022) [MEDLINE]: n = 175 (57.5 ± 17.1 y/o)
- Approximately 44% of Patients Had Early-Onset Asthma and 56% of Patients Had Late-Onset Asthma
- Comorbidities Had a Differential Impact in the Two Groups
- Rhinitis was More Frequent in Early-Onset Asthma (76 vs 53%; p = 0.02) and was Associated with Uncontrolled Asthma (p<0.001), Decreased FEV1/FVC Ratio (p = 0.01), Increased Eosinophils (p = 0.003) and Total IgE (p <0.01)
- Conversely, in Late-Onset Asthma, Rhinitis was Associated with More Controlled Asthma and Higher FEV1/FVC (Both p < 0.01)
- In Early-Onset Asthma, Only IgE Levels were Directly Related to Blood Eosinophils (r = 0.42; p< 0.001) and Inversely Related to FEV1/FVC Ratio (r = -0.35; p= 0.002)
- Obesity was Present in 20% of Patients in Both Groups
- However, Only in Late-Onset Asthma was Obesity Associated with Uncontrolled Disease (p = 0.009), Decreased FEV1/FVC Ratio (p = 0.009) and Blood Neutrophils (p = 0.03)
- In Multivariable Regression Analysis, Rhinitis in Early-Onset Asthma and Obesity in Late-Onset Asthma were the Risk Factor Most Closely Associated with Poor Control
- Gastroesophageal Reflux Disease (GERD), Cardiovascular Disease, and Bronchiectasis Did Not Affect Control
- Early-Onset Persistent and Late-Onset Asthma are Distinct Phenotypes, with Different Inflammatory Patterns and Different Comorbidities Which Impact on Symptom Control
- Approximately 44% of Patients Had Early-Onset Asthma and 56% of Patients Had Late-Onset Asthma
- Adolescents/Adults Who Present with “New-Onset” Asthma Symptoms May Have a History of Asthma Symptoms or Diagnosis in Childhood (NEJM, 2003) [MEDLINE]
- Specific Subtypes of Asthma Which Typically Exhibit Onset in Adulthood
- Aspirin-Exacerbated Respiratory Disease (AERD) (see Aspirin-Exacerbated Respiratory Disease)
- Previously Referred to as “Aspirin-Sensitive Asthma”
- Eosinophilic Asthma
- Eosinophilic/T2-High Phenotype Appears More Commonly in Late-Onset Severe Asthma than in Childhood-Onset Severe Asthma (Which is More Typically Associated with Atopy)
- Occupational Asthma (see Occupational Asthma)
- Aspirin-Exacerbated Respiratory Disease (AERD) (see Aspirin-Exacerbated Respiratory Disease)
Historical Features
- Pattern of Respiratory Symptoms Which Occur Following Exposure to Various Triggers (Such as Allergens, Exercise, Viral Respiratory Infection, etc) and Resolve with Trigger Avoidance or Asthma Medication is Typical of Asthma
- However, the Diagnosis of Asthma is Difficult Based on History Alone (JAMA, 2017) [MEDLINE]
- Historical Features Which Increase the Diagnostic Probability of Asthma
- Episodic Symptoms
- Typically Fluctuating Over Hours-Days
- Resolving with Removal of a Trigger and/or Use of an Asthma Medication
- Worsening During the Nighttime (Frequent in Asthma)
- Characteristic Triggers
- Aeroallergens (Dust Mites, Mold/Mold Spores, Furry Animals, Cockroaches, or Pollen)
- Cold Air
- Exercise (Typically within 5-15 min After a Brief Exertion or 15 min into a Prolonged Exertion; Typically Resolving After 30-60 min of Rest)
- History of Asthmatic Symptoms in Childhood
- Personal/Family History of Atopy (Atopic Dermatitis, Seasonal/Perennial Allergic Rhinitis and/or Conjunctivitis)
- In Patient with Exertional Dyspnea, Cough, or Wheeze, the Presence of Atopy Makes Asthma More than Chronic Obstructive Pulmonary Disease (COPD) (J Investig Allergol Clin Immunol, 2006) [MEDLINE]
- Work-Related Exposure
- Approximately 10% of of New-Onset Adult Asthma Cases are Due to Workplace-Related Exposures (i.e. Occupational Asthma)
- Episodic Symptoms
- Historical Features Which Decrease the Diagnostic Probability of Asthma
- Concomitant Cardiovascular Symptoms (Chest Pain, Lightheadedness, Syncope, Palpitations, etc)
- History of Cigarette Smoking for Multiple Years
- Lack of Improvement After Use of Asthma Medications
- Onset of Symptoms After Age 50
Severe Asthma Phenotypes
- Type 2 Asthma Phenotypes: approximately 70% of patients with severe asthma have evidence of high levels of T2 inflammation (T2-high)
- Childhood-Onset Type 2 Asthma
- Adult-Onset Type 2 Asthma
- Hypereosinophilic Adult-Onset Asthma with Extrapulmonary Disease
- Aspirin-Exacerbated Respiratory Disease (AERD) (see Aspirin-Exacerbated Respiratory Disease)
- Chronic Rhinosinusitis with Nasal Polyposis
- Eosinophilic Granulomatosis with Polyangiitis (EGPA) (see xxxx)
- Asthmatic Granulomatosis
- Some patients with severe asthma have granulomatous inflammation on lung biopsy that is not related to eosinophilic granulomatosis with polyangiitis
- It is unknown whether this inflammation is an intercurrent disease process, a consequence of therapy, or a different asthma phenotype
- Non-Type 2 Asthma Phenotypes
- IL-6/obesity-Associated Asthma
- Neutrophilic Asthma
- Paucigranulocytic Asthma
- Perimenopausal-Onset Asthma
- Complex Combined Type 1 and Type 2 Asthma
Stability of Asthma Severity
- In Cohort Studies Which Have Studied Asthma Over 5-25 Years, Asthma Severity Appears to Remain Stable Over Several Years (Ann Allergy Asthma Immunol, 2000) [MEDLINE] (Am J Med, 2002) [MEDLINE] (Allergy, 2020) [MEDLINE]
- It is Unclear if Corticosteroids/Other Biologic Therapies Can Decrease Airway Remodeling and Alter the Natural History of Asthma in Adults (Clin Chest Med, 2000) [MEDLINE]
Rate of Decline of Lung Function in Asthma
- Asthma Patients Manifest a More Rapid Rate of Decline in Lung Function than Do Normal Patients (NEJM, 1998) [MEDLINE] (Eur Respir J, 2007) [MEDLINE] (Am J Respir Crit Care Med, 2023) [MEDLINE]
- Rate of Decline in Lung Function is Associated with Asthma Severity
- Patients with the Most Severe Asthma Symptoms Have the Most Rapid Rate of Decline in the Forced Expiratory Volume in 1 Sec (FEV1)/Forced Vital Capacity (FVC) Ratio, as Compared to Control Patients and Asthma Patients with Less Severe Disease (Am Rev Respir Dis, 1988) [MEDLINE]
- Rate of Decline in Lung Function Appears to Be Higher in the Setting of New-Onset Asthma
- Rate of Decline in Lung Function is Accelerated by Cigarette Smoke Exposure
- Cigarette Smoking Accelerates the Rate of Decline in Lung Function in Asthma Patients (NEJM, 1998) [MEDLINE]
Remission of Asthma
- While Asthma is a Common Disease in Childhood, Many Children (Particularly Males) Exhibit a Remission of Asthma Symptoms Around the Time of Puberty (with a Potential Recurrence of Their Asthma Years Later)
- *Adults are Less Likely to Experience a Complete Remission of Asthma Symptoms than Children (Chest, 1986) [MEDLINE] (Am J Med, 2002) [MEDLINE]
Comorbid Conditions Which May Exacerbate Asthma Symptoms and Influence Asthma Control
- Allergic Bronchopulmonary Aspergillosis (ABPA) (see Allergic Bronchopulmonary Aspergillosis)
- Epidemiology
- Allergic Bronchopulmonary Aspergillosis is Present in 2-32% of Asthmatics (Int J Tuberc Lung Dis, 2009) [MEDLINE]
- Diagnosis
- Aspergillus Fumigatus-Specific Antibodies
- Elevated Serum IgA (see see Serum Immunoglobulin A)
- Elevated Serum IgE (see Serum Immunoglobulin E)
- Peripheral Eosinophilia (see Peripheral Eosinophilia)
- Positive Skin Test to *Aspergillus Fumigatus
- Precipitating Antibodies Against Aspergillus Fumigatus Antigen
- Clinical
- Asthma-Like Presentation
- Central Bronchiectasis (see Bronchiectasis)
- Epidemiology
- Allergic Rhinitis (see Allergic Rhinitis)
- Epidemiology
- Common in the Setting of Allergic Asthma
- Clinical
- Cobblestone Appearance of the Posterior Pharyngeal Wall
- Pale, Swollen Nasal Membranes
- Epidemiology
- Aspirin-Exacerbated Respiratory Disease (AERD) (see Aspirin-Exacerbated Respiratory Disease)
- Epidemiology
- Aspirin-Exacerbated Respiratory Disease is Present in Approximately 7.15% of Typical Adult Asthma Patients and Approximately 14.89% of Patients with Severe Asthma (J Allergy Clin Immunol, 2015) [MEDLINE]
- Aspirin-Exacerbated Respiratory Disease (AERD) is Usually Diagnosed in Adulthood
- Diagnosis
- Aspirin Challenge is the Only Definitive Means of Diagnosing Aspirin-Exacerbated Respiratory Disease
- Clinical Manifestations
- Asthma (see Asthma)
- Chronic Rhinosinusitis with Nasal Polyposis
- Reaction to Aspirin and Other COX-1 Inhibiting Nonsteroidal Anti-Inflammatory Drugs (NSAID’s)
- With Clinical Symptoms of Nasal Congestion and Bronchoconstriction Beginning 20-180 min After Exposure
- Epidemiology
- Depression/Chronic Stress (see Depression)
- Epidemiology
- XXX
- Epidemiology
- Asthma-Chronic Obstructive Pulmonary Disease (COPD) Overlap (ACO) (Concomitant Asthma-Chronic Obstructive Pulmonary Disease)
- Epidemiology
- No Universally Accepted Definition Exists for Asthma-Chronic Obstructive Pulmonary Disease (COPD) Overlap (ACO)
- Therefore, Instead of Asthma-Chronic Obstructive Pulmonary Disease (COPD) Overlap (ACO), the Global Initiative for Asthma (GINA) and the Global Initiative for Obstructive Lung Disease (GOLD) Use the Terminology “Coexisting” or “Concomitant” Asthma and Chronic Obstructive Pulmonary Disease (COPD) in Their Reports
- Epidemiology
- Gastroesophageal Reflux Disease (GERD) (see Gastroesophageal Reflux Disease)
- Epidemiology
- XXX
- Epidemiology
- Inducible Laryngeal Obstruction (Vocal Cord Dysfunction) (see Inducible Laryngeal Obstruction)
- Epidemiology
- Up to 75% of Asthma Patients Have Coexistent Inducible Laryngeal Obstruction (Vocal Cord Dysfunction)
- Diagnosis
- Flexible Laryngoscopy (see Flexible Laryngoscopy)
- Clinical
- XXXXX
- Epidemiology
- Obesity with/without Type 2 Diabetes (see Obesity and Diabetes Mellitus)
- Epidemiology
- XXXX
- Clinical
- XXXXX
- Epidemiology
- Obstructive Sleep Apnea (OSA) (see Obstructive Sleep Apnea)
- Epidemiology
- XXXX
- Clinical
- XXXXX
- Epidemiology
- Rhinosinusitis with/without Nasal Polyps
- Epidemiology
- XXXX
- Clinical
- XXXXX
- Epidemiology
- Social Determinants of Health
- Increased Exposure to Air Pollution
- Lack of Access to Medications/Medical Care
- Poor Housing Conditions
Infectious Manifestations
Risk of Bacterial Respiratory Infection
- Epidemiology
- XXXX
- Clinical
- XXXXX
Risk of Viral Respiratory Infection
- Epidemiology
- Influenza Virus (see Influenza Virus)
- Respiratory Syncytial Virus (RSV) (see Respiratory Syncytial Virus)
- Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2, COVID-19) (see Severe Acute Respiratory Syndrome Coronavirus-2)
- Acquisition
- Asthma Does Not Increase the Risk of Acquiring Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2, COVID-19) (Global Initiative for Asthma, Global Strategy for Asthma Management and Prevention, Updated 2022) [MEDLINE]
- Severity of Infection
- Patients with Well-Controlled Asthma Do Not Have an Increased Risk of SARS-CoV-2 Infection-Related Death (Global Initiative for Asthma, Global Strategy for Asthma Management and Prevention, Updated 2022) [MEDLINE]
- However, the Risk of SARS-CoV-2 Infection-Related Death is Increased in Asthma Patients WHo Have Recently Required Oral Corticosteroids for Their Asthma (Global Initiative for Asthma, Global Strategy for Asthma Management and Prevention, Updated 2022) [MEDLINE]
- Acquisition
Neurologic Manifestations
Circadian Rhythm Disruption
- Epidemiology
- XXX
- Association of rest-activity circadian rhythm with chronic respiratory diseases, a cross-section survey from NHANES 2011-2014. Respir Med. 2023 Feb 6;209:107147. doi: 10.1016/j.rmed.2023.107147 [MEDLINE]
- A total of 7412 participants from the National Health and Nutrition Examination Survey (NHANES) 2011-2014 were included in this study. The rest-activity circadian rhythm indices were calculated using accelerometer data and were divided into quartiles to perform logistic regression.
- Results: Participants in the highest quartile of Relative amplitude (RA) had a lower prevalence of emphysema, chronic bronchitis and asthma, compared to those in the lowest quartile. Participants in the highest quartile of Intradaily variability (IV) was associated with a higher prevalence of emphysema relative to those in the lowest quartile. Compared to those in the lowest quartile, participants in the highest quartile of the average activity of the most active continuous 10-h period (M10) had a lower prevalence of emphysema. Additionally, compared to those in the lowest quartile of the average activity of the least active continuous 5-h period (L5) and L5 start time, participants in the highest quartile had a higher prevalence of asthma.
- Conclusions: This study demonstrated that in general US adult population, disrupted rest-activity circadian rhythm was associated with a higher prevalence of chronic respiratory diseases
Otolayngologic Manifestations
Paradoxical Vocal Fold Motion (Vocal Cord Dysfunction) (see Paradoxical Vocal Fold Motion)
- Epidemiology
- Up to 75% of Asthma Patients Have Coexistent Vocal Cord Dysfunction
- Diagnosis
- Flexible Laryngoscopy (see Flexible Laryngoscopy)
- Management
- XXXX
Pulmonary Manifestations
Allergic Bronchopulmonary Aspergillosis (ABPA) (see Allergic Bronchopulmonary Aspergillosis)
- Epidemiology
- Allergic Bronchopulmonary Aspergillosis is Present in 2-32% of Asthmatics (Int J Tuberc Lung Dis, 2009) [MEDLINE]
- Diagnostic Features
- Aspergillus Fumigatus-Specific Antibodies
- Asthma-Like Presentation
- Central Bronchiectasis (see Bronchiectasis)
- Elevated Serum IgA (see see Serum Immunoglobulin A)
- Elevated Serum IgE (see Serum Immunoglobulin E)
- Peripheral Eosinophilia (see Peripheral Eosinophilia)
- Positive Skin Test to *Aspergillus Fumigatus
- Precipitating Antibodies Against Aspergillus Fumigatus Antigen
Cough (see Cough)
- Epidemiology
- XXXX
Dyspnea (see Dyspnea)
- Epidemiology
- XXXX
Severe Asthma with Fungal Sensitization (SAFS)
- Epidemiology
- Subgroup of Asthmatics
- Clinical
- Severe Asthma
- ATS Definition of Severe Asthma: need for oral steroids ≥50% of time and need for high-dose inhaled steroid (belcomethasone ≥1200 mg/day or equivalent) and ≥1 other controller (e.g. long-acting bronchodilator, montelukast, etc.) to achieve control at level of mild persistent asthma
- Positive Immediate Skin Test or In Vitro Specific IgE to ≥1 Filamentous Fungi
- Exclusion of Allergic Bronchopulmonary Aspergillosis (ABPA) (see Allergic Bronchopulmonary Aspergillosis)
- SAFS patients do not meet the necessary constellation of clinical, serological and radiological criteria for a diagnosis of ABPA, usually because total IgE levels are <1000 IU/mLand/or key radiographic findings, such as mucoid impaction or bronchiectasis, are lacking
- Severe Asthma
Other Manifestations
- xxxx
Asthma in Pregnancy (see Pregnancy)
- Epidemiology
- Uncontrolled Asthma Increases the Risk of Perinatal Mortality, Pre-Eclampsia, Preterm Birth, and Low Birthweight Infant
- Asthma Improves in 33% of Women, Worsens in 33% of Women, and Stays the Same in 33% of Women
- Physiology
- Asthma May Improve in Approximately 33% of Cases During Pregnancy, Due Predominantly to Progesterone-Induced Bronchodilation and Increased Circulating Histaminase
- Diagnosis
1) ABG: pCO2 is usually <35 with slight metabolic acidosis (pH ranges from 7.4-7.45) and normal pO2 a) Increased VE (begins during first trimester, up to 48% increase by term) with Normal-Mildly Elevated RR: due to progesterone b) Increased VT (30-35% above normal, to around 450-600 ml) with Increased A-P Diameter of Chest 2) Swan: a) PVR decreased (up to 35% by late pregnancy): b) Increased CO and blood volume with normal PCWP and CVP 3) PFT s/Exercise Testing: a) FRC and RV are decreased (with preserved FEV1 and VC) b) Increased oxygen consumption (rises to 40-100% above normal) + Increased CO2 Production (rises to 30-50% above normal by third trimester)
- Clinical
- Dyspnea (see Dyspnea)
- Dyspnea is Common in All Pregnancies: due to progesterone secreted by the placenta
- Dyspnea (see Dyspnea)
Specific Clinical Manifestations of Acute Asthma Exacerbation
Epidemiology
- XXXXX
- International variation in severe exacerbation rates in patients with severe asthma. Chest. Published online February 21, 2024. doi:10.1016/j.chest.2024.02.029 [MEDLINE]
- Background: Exacerbation frequency strongly influences treatment choices in patients with severe asthma
- Research question: What is the extent of the variability of exacerbations rate across countries and its implications in disease management?
- Study design and methods: We retrieved data from the International Severe Asthma Registry, an international observational cohort of patients with a clinical diagnosis of severe asthma. We identified patients aged ≥18 years who did not initiate any biologics prior to baseline visit. A severe exacerbation was defined as the use of oral corticosteroids for ≥3 days or asthma-related hospitalization/emergency room visit. A series of negative binomial models were applied to estimate country-specific severe exacerbation rates during 365 days of follow-up, starting from a naïve model with country as the only variable, to an adjusted model with country as a random-effect term and patient and disease characteristics as independent variables
- Results: The final sample included 7,510 patients from 17 countries (56% from the United States), contributing to 1,939 severe exacerbations (0.27/person-year). There was large between-country variation in observed severe exacerbation rate (min: 0.04 [Argentina], max:0.88 [Saudi Arabia], interquartile range [IQR]: 0.13-0.54), which remained substantial after adjusting for patient characteristics and sampling variability (IQR: 0.16-0.39)
- Interpretation: Individuals with similar patient characteristics but coming from different jurisdictions have varied severe exacerbation risks, even after controlling for patient and disease characteristics. This suggests unknown patient factors or system-level variations at play. Disease management guidelines should recognize such between-country variability. Risk prediction models that are calibrated for each jurisdiction will be needed to optimize treatment strategies.
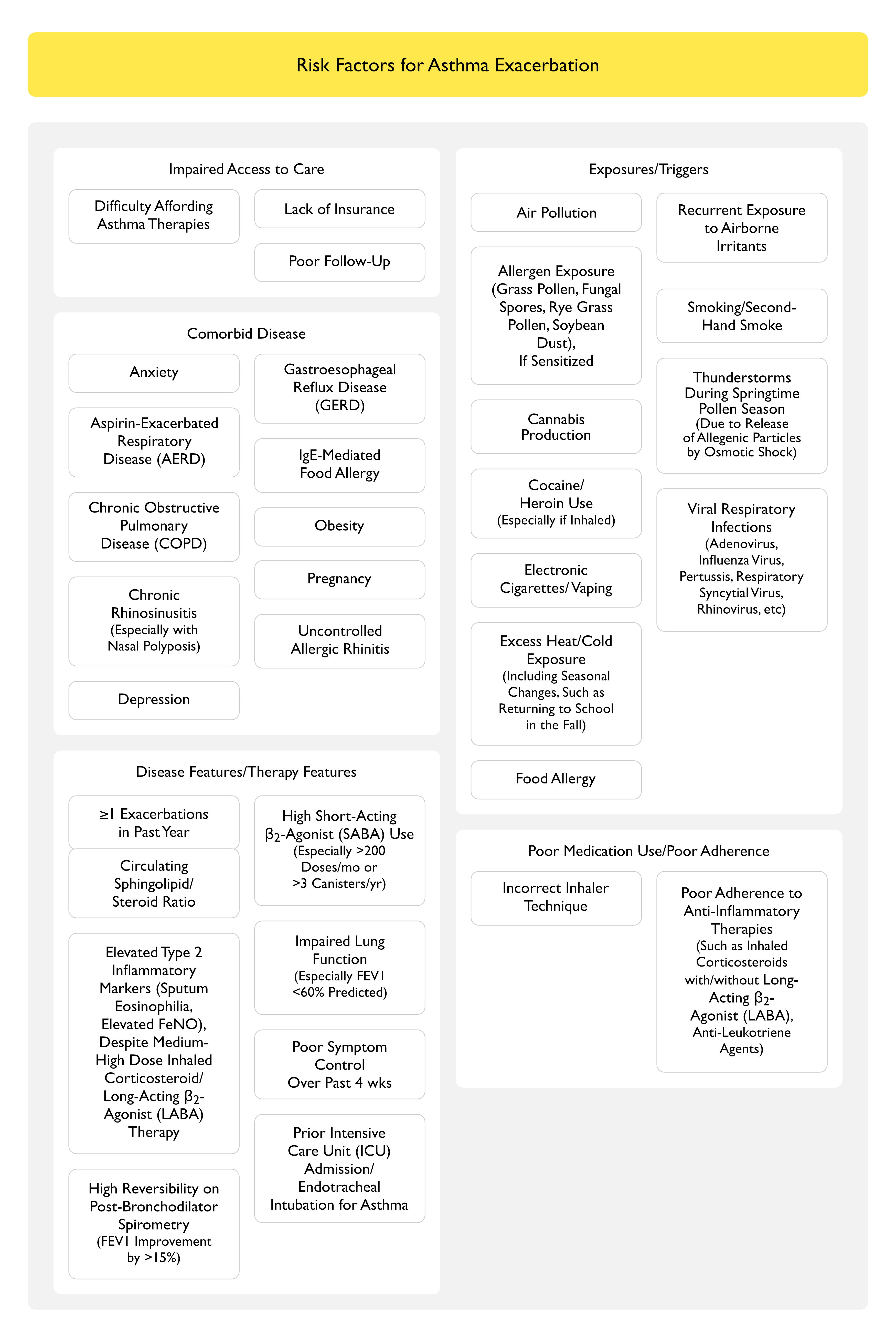
Risk Factors of Asthma Exacerbation
Clinical Classification of Asthma Exacerbation in the Emergency Department (GINA, 2025)
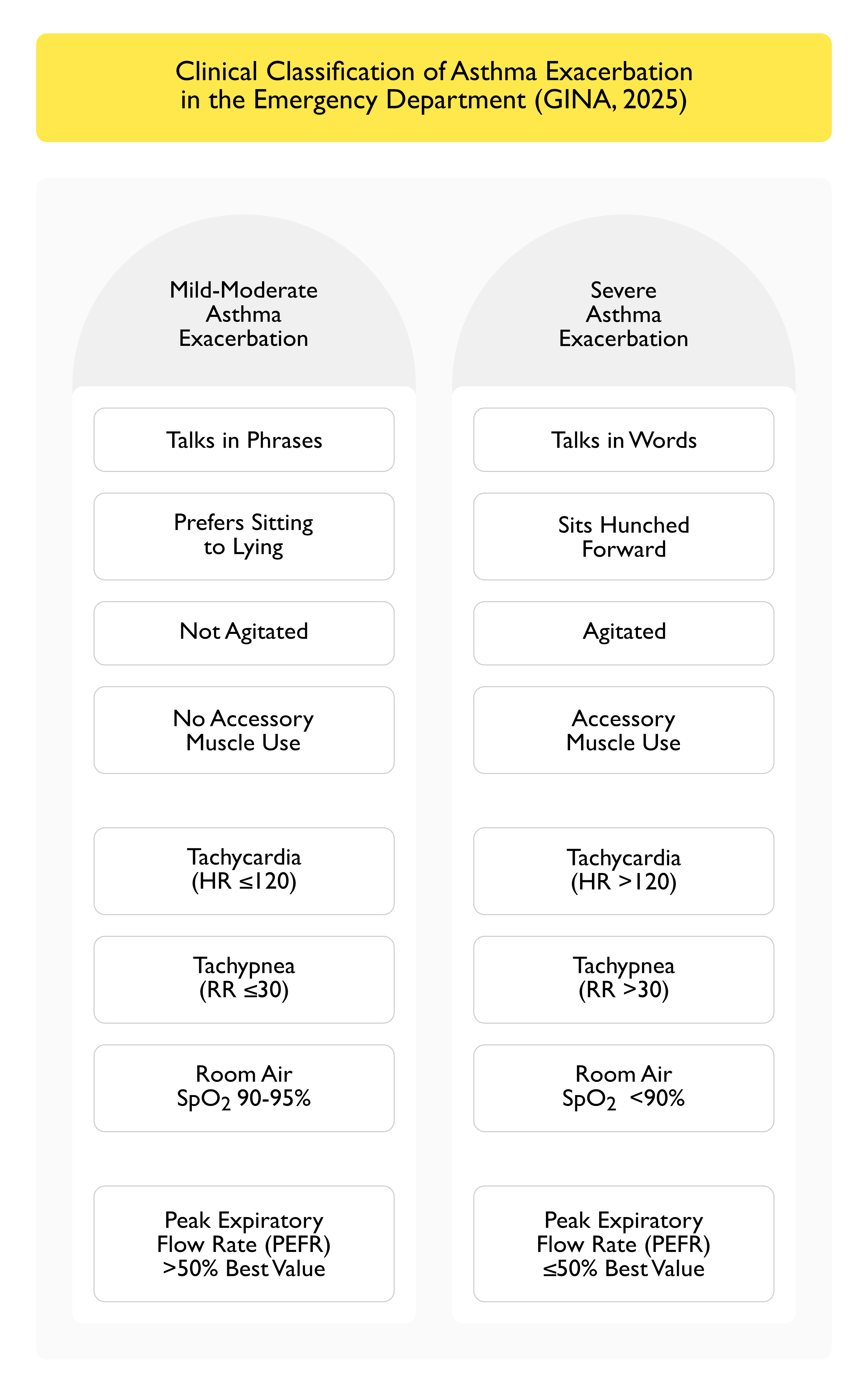
- Mild-Moderate Asthma Exacerbation
- Talks in Phrases
- Prefers Sitting to Lying
- Not Agitated
- No Accessory Muscle Use
- Tachycardia (HR ≤120)
- Tachypnea (RR ≤30)
- Room Air SpO2 90-95%
- Peak Expiratory Flow Rate (PEFR) >50% Best Value
- Severe Asthma Exacerbation
- Talks in Words
- Sits Hunched Forward
- Agitated
- Accessory Muscle Use
- Tachycardia (HR >120)
- Tachypnea (RR >30)
- Room Air SpO2 <90%
- Peak Expiratory Flow Rate (PEFR) ≤50% Best Value
Clinical Features
- General Comments
- Some Patients are Very Sensitive to an Increase in Asthma Symptoms, While Other Patients Perceive Decreased Airflow Only When it Becomes Severe
- Anxiety/Agitation (see Anxiety and Agitation)
- May Occur in Severe Asthma Exacerbation
- Chest Tightness
- Common
- Cough (see Cough)
- Common
- May Be Intractable in Severe Asthma Exacerbation
- Decreased Exercise Tolerance
- Decreased Peak Expiratory Flow Rate (PEFR)
- Decreased Peak Expiratory Flow Rate (PEFR) May Be the First Sign that Asthma Control is Deteriorating
- Since Normal Peak Expiratory Flow Rate (PEFR) Varies with Age, Sex, and Height, Each Patient Needs to Establish Their Own Baseline Value, to Which Readings During an Exacerbation Can Be Compared
- Decrease in Peak Expiratory Flow Rate (PEFR) of >20 % from Normal (or from the Patient’s Personal Best) Indicates the Presence of an Asthma Exacerbation
- Decrease in Peak Expiratory Flow Rate (PEFR) of ≥50 % from Normal (or from the Patient’s Personal Best) Indicates the Presence of a Severe Asthma Exacerbation
- Decreased Peak Expiratory Flow Rate (PEFR) Provides an Estimate of the Severity of the Asthma Exacerbation
- Degree of Decrease in the Peak Expiratory Flow Rate (PEFR) May Be Useful to Determine the Appropriate Site of Care (Home, Outpatient Office, or Emergency Department)
- Decreased Peak Expiratory Flow Rate (PEFR) May Be Especially Useful in Patients Who May Not Perceive Decreased Airflow Until it Becomes Severe
- Dyspnea (see Dyspnea)
- Common
- Due to Decreased Expiratory Airflow Rate, Gas Trapping, Hyperinflation, V/Q Mismatch, etc
- Fatigue (see Fatigue)
- Common
- Inability to Lie Supine
- May Occur in Severe Asthma Exacerbation
- Pneumomediastinum/Pneumothorax (see Pneumomediastinum and Pneumothorax)
- XXXX
- Prolonged Expiratory Phase
- May Accompany Wheezing
- Pulsus Paradoxus (see Pulsus Paradoxus)
- Defined as a Decrease of >10 mm Hg in Systolic Blood Pressure During Inspiration
