Etiology of Absolute Anemia (Decreased RBC Volume)
Decreased RBC Production
Hereditary
- Erythroid Progenitor Cell Failure
- Congenital Dyserythropoietic Syndromes
- Diamond-Blackfan Syndrome
- Functional Impairment of Erythroid and Other Progenitors
- Selective Malabsorption of Vitamin B12 (Imerslund-Gräsbeck disease)
- Congenital Intrinsic Factor Deficiency
- Transcobalamin II Deficiency
- Inborn Errors of Cobalamin Metabolism
- Methylmalonic Aciduria
- Homocystinuria
- Inborn Errors of Folate Metabolism
- Congenital Folate Malabsorption
- Dihydrofolate Deficiency
- Methyltransferase Deficiency
- Inborn Purine and Pyrimidine Metabolism Defects
- Lesch-Nyhan Syndrome
- Hereditary Orotic Aciduria
- Inborn Errors of Iron Metabolism
- Hereditary Atransferrinemia
- Hypochromic Anemia Associated with Divalent Metal Transporter (DMT)-1 Mutation
- Hereditary Sideroblastic Anemia
- X Chromosome-Linked: ALAS2 deficiency, Hereditary Sideroblastic Anemia with Ataxia: mitochondrial ATP binding cassette (ABCB7) mutations
- Autosomal: Mitochondrial Myopathy and Sideroblastic Anemia (PSU1 mutations)
- Mitochondrial: Pearson Marrow-Pancreas Syndrome
- Thalassemias (see Thalassemia, [[Thalassemia]])
- Alpha Thalassemia
- Beta Thalassemia
- Hemoglobin Constant Spring
- Hemoglobin E
- Hemoglobin Lepore
- Pluripotent Stem Cell Failure
- Dyskeratosis Congenita
- Fanconi Anemia
- Shwachman-Diamond Syndrome (aka Shwachman–Bodian–Diamond Syndrome)
Acquired
- Erythroid Progenitor Cell Failure
- Acquired Sideroblastic Anemia
- Primary Sideroblastic Anemia (see myelodysplastic syndromes)
- Subunit 1 of the Mitochondrial Cytochrome Oxidase
- Secondary Sideroblastic Anemia
- Chloramphenicol
- Copper Deficiency (see Copper, [[Copper]])
- Chronic Neoplastic and Inflammatory Disease
- Cycloserine (see Cycloserine, [[Cycloserine]])
- Ethanol (see Ethanol, [[Ethanol]])
- Isoniazid (see Isoniazid, [[Isoniazid]])
- Lead (see Lead, [[Lead]])
- Pyrazinamide (see Pyrazinamide, [[Pyrazinamide]])
- Zinc Ingestion (see Zinc, [[Zinc]])
- Primary Sideroblastic Anemia (see myelodysplastic syndromes)
- Endocrine Disease
- Hypothyroidism (see Hypothyroidism, [[Hypothyroidism]])
- Hyperthyroidism (see Hyperthyroidism, [[Hyperthyroidism]])
- Adrenal Insufficiency (see Adrenal Insufficiency, [[Adrenal Insufficiency]])
- Cushing Syndrome (see Cushing Syndrome, [[Cushing Syndrome]])
- Androgen Deficiency (see Hypotestosteronemia, [[Hypotestosteronemia]])
- Panhypopituitarism (see Panhypopituitarism, [[Panhypopituitarism]])
- Hyperparathyroidism (see Hyperparathyroidism, [[Hyperparathyroidism]])
- Pure Red Cell Aplasia (see Pure Red Cell Aplasia, [[Pure Red Cell Aplasia]])
- Acquired Sideroblastic Anemia
- Functional Impairment of Erythroid and Other Progenitors
- Acquired Thalassemia: manifests as hemoglobin H disease or mild -thalassemia
- Common Variable Immunodeficiency (CVID) (see Common Variable Immunodeficiency, [[Common Variable Immunodeficiency]])
- Myelodysplastic Syndrome (see Myelodysplastic Syndrome, [[Myelodysplastic Syndrome]])
- Myeloid Leukemia: may occur in elderly patients
- Anemia of Chronic Disease/Anemia of Inflammation (see Anemia of Chronic Disease, [[Anemia of Chronic Disease]])
- Anemia of Chronic Kidney Disease (see Chronic Kidney Disease, [[Chronic Kidney Disease]])
- Anemia of Chronic Liver Disease (see End-Stage Liver Disease, [[End-Stage Liver Disease]])
- Anemia of Starvation
- Copper Deficiency (see Copper, [[Copper]])
- Drug-Induced Megaloblastic Anemia
- Methotrexate (see Methotrexate, [[Methotrexate]])
- Pemetrexed (see Pemetrexed, [[Pemetrexed]])
- Phenytoin Toxicity (see Phenytoin, [[Phenytoin]])
- Erythropoietin Antibodies
- Ethanol Abuse (see Ethanol, [[Ethanol]])
- Folate Deficiency (see Folate, [[Folate]])
- Iron Deficiency Anemia (see Iron, [[Iron]] and Iron Deficiency Anemia, [[Iron Deficiency Anemia]])
- Lead Intoxication (see Lead, [[Lead]])
- Niacin Deficiency (see Niacin, [[Niacin]])
- Nitrous Oxide
- Panthothenic Acid Deficiency
- Protein Deficiency (Kwashiorkor)
- Riboflavin Deficiency
- Selenium Deficiency (see Selenium, [[Selenium]])
- Thiamine Deficiency
- Vitamin A Deficiency
- Vitamin B6 Deficiency
- Vitamin B12 Deficiency
- Vitamin C Deficiency
- Vitamin E Deficiency
- Zinc Deficiency (see Zinc, [[Zinc]])
- Acquired Thalassemia: manifests as hemoglobin H disease or mild -thalassemia
- Pluripotent Stem Cell Failure
- Pancytopenia with Hypocellular Bone Marrow (see Pancytopenia, [[Pancytopenia]])
- Aplastic Anemia (see Aplastic Anemia, [[Aplastic Anemia]])
- Other
- Acute Lymphocytic Leukemia (ALL) (see Acute Lymphocytic Leukemia, [[Acute Lymphocytic Leukemia]]): some cases
- Aleukemic Leukemia
- Lymphoma (see Lymphoma, [[Lymphoma]]): involving bone marrow
- Myelodysplastic Syndrome (see Myelodysplastic Syndrome, [[Myelodysplastic Syndrome]])
- Pancytopenia with Cellular Bone Marrow (see Pancytopenia, [[Pancytopenia]])
- Bone Marrow Infiltration (see Pancytopenia, [[Pancytopenia]])
- Malignancy
- Infection
- Macrophages
- Bone Marrow Necrosis
- Other
- Myelofibrosis/Myelophthisis (see Pancytopenia, [[Pancytopenia]])
- Malignancy
- Infection
- Macrophages
- Bone Marrow Necrosis
- Other
- Other
- Ethanol (see Ethanol, [[Ethanol]])
- Folate Deficiency (see Folate, [[Folate]])
- Hypersplenism (see Splenomegaly, [[Splenomegaly]])
- Vitamin B12 Deficiency (see Vitamin B12, [[Vitamin B12]])
- Bone Marrow Infiltration (see Pancytopenia, [[Pancytopenia]])
- Hypocellular Bone Marrow with/without Pancytopenia (see Pancytopenia, [[Pancytopenia]])
- Anorexia Nervosa
- Legionellosis (see Legionellosis, [[Legionellosis]])
- Mycobacterium Avium-Intracellulare (MAI) (see Mycobacterium Avium-Intracellulare, [[Mycobacterium Avium-Intracellulare]])
- Q Fever (see Q Fever, [[Q Fever]])
- Starvation
- Tuberculosis (see Tuberculosis, [[Tuberculosis]])
- Pancytopenia with Hypocellular Bone Marrow (see Pancytopenia, [[Pancytopenia]])
Increased RBC Destruction
Hereditary
- Familial Atypical Hemolytic-Uremic Syndrome (aHUS) (see Hemolytic-Uremic Syndrome, [[Hemolytic-Uremic Syndrome]])
- Hemoglobinopathies
- Sickle Cell Disease (see Sickle Cell Disease, [[Sickle Cell Disease]])
- Unstable Hemoglobins
- RBC Cell Membrane Defect
- Cytoskeletal Membrane Defect
- Hereditary Spherocytosis (see Hereditary Spherocytosis, [[Hereditary Spherocytosis]])
- Hereditary Elliptocytosis (see Hereditary Elliptocytosis, [[Hereditary Elliptocytosis]])
- Pyropoikilocytosis
- Lipid Membrane Disorders
- Hereditary Abetalipoproteinemia
- Hereditary Stomatocytosis
- Membrane Disorders Associated with Abnormalities of Erythrocyte Antigens
- McLeod Syndrome
- Rh Deficiency Syndromes
- Membrane Disorders Associated with Abnormal Transport
- Hereditary Xerocytosis
- Cytoskeletal Membrane Defect
- RBC Enzyme Defects
- Glycolytic
- Aldolase Deficiency
- Diphosphoglycerate Mutase (DPGM) Deficiency
- Glucose-6-Phosphate Isomerase (G6PI) Deficiency
- Glyceraldehyde-3-Phosphate Dehydrogenase (GAPD) Deficiency
- Hexokinase Deficiency
- Phosphofructokinase (PFK) Deficiency
- Phosphoglycerate Kinase (PGK) Deficiency
- Pyruvate Kinase (PK) Deficiency
- Triose Phosphate Isomerase (TPI) Deficiency
- Redox
- Cytochrome B5 Reductase Deficiency
- Gamma Glutamylcysteine Synthase Deficiency
- Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency (see Glucose-6-Phosphate Dehydrogenase Deficiency, [[Glucose-6-Phosphate Dehydrogenase Deficiency]])
- Glutathione Synthase Deficiency
- Nucleotide Metabolism
- Adenylate Kinase Deficiency
- Pyrimidine 5′-Nucleotidase
- Glycolytic
- Porphyrias
- Congenital Erythropoietic and Hepatoerythropoietic Porphyrias
- Congenital Erythropoietic Protoporphyria
Acquired
- Antibody-Mediated Hemolytic Anemia
- Acute Hemolytic Transfusion Reaction (see Acute Hemolytic Transfusion Reaction, [[Acute Hemolytic Transfusion Reaction]])
- Autoimmune Hemolytic Anemia (AIHA) (see Autoimmune Hemolytic Anemia, [[Autoimmune Hemolytic Anemia]])
- Cryopathic Syndromes
- Cold Agglutinin Disease
- Paroxysmal Cold Hemoglobinuria (see Paroxysmal Cold Hemoglobinuria, [[Paroxysmal Cold Hemoglobinuria]])
- Cryoglobulinemia (see Cryoglobulinemia, [[Cryoglobulinemia]])
- Delayed Hemolytic Transfusion Reaction (see Delayed Hemolytic Transfusion Reaction, [[Delayed Hemolytic Transfusion Reaction]])
- Chemical Injury to RBC: these agents may cause hemolysis, even in absence of G6PD deficiency
- Arsenic (see Arsenic, [[Arsenic]])
- Arsine Vapor (see Arsine, [[Arsine]])
- Brown Recluse Spider Bite (Loxoscelism) (see Brown Recluse Spider Bite, [[Brown Recluse Spider Bite]])
- Copper (see Copper, [[Copper]])
- Chlorate
- Cisplatin (see Cisplatin, [[Cisplatin]])
- Dapsone (see Dapsone, [[Dapsone]])
- Hyperbaric Oxygen/100% Oxygen
- Jequirity Bean
- Lead (see Lead, [[Lead]])
- Mercury
- Methylene Blue (see Methylene Blue, [[Methylene Blue]])
- Nitrates (see Nitrites and Nitrates, [[Nitrites and Nitrates]])
- Saponin Plant Extracts (see [[]])
- Scorpion Bite (see Scorpion Bite, [[Scorpion Bite]])
- Snake Venom (cobra, viper)
- Stibine
- Hypersplenism (see Splenomegaly, [[Splenomegaly]])
- Mechanical RBC Destruction
- Macroangiopathic Hemolytic Anemia
- Cardiac Hemolysis: asscoiated with prosthetic heart valves, prosthetic patch, calcific AS, aorto-femoral bypass, ruptured chordae tendinae, aortic coarctation, aortic aneurysm
- March Hemoglobinuria
- Microangiopathic Hemolytic Anemia (MAHA)
- Bevacizumab (Avastin) (see Bevacizumab, [[Bevacizumab]])
- Disseminated Intravascular Coagulation (DIC) (see Disseminated Intravascular Coagulation, [[Disseminated Intravascular Coagulation]])
- Thrombocytopenia
- Hemolysis is varable
- Less severe than TTP usually
- Giant Hemangioma (Kasabach-Merritt Syndrome) (see Kasabach-Merritt Syndrome, [[Kasabach-Merritt Syndrome]])
- Abnormal vessel wall -> damage to RBC
- Mild thrombocytopenia
- HELLP Syndrome (see HELLP Syndrome, [[HELLP Syndrome]])
- Hemolytic-Uremic Syndrome (see Hemolytic-Uremic Syndrome, [[Hemolytic-Uremic Syndrome]])
- Malignant Hypertension (see Malignant Hypertension, [[Malignant Hypertension]])
- Abnormal vessel wall -> damage to RBC
- Mild thrombocytopenia
- Metastatic Carcinoma: due to activation of multifocal clotting -> hemolysis and thrombocytopenia
- Multiple Pulmonary Metastases from Adenocarcinoma
- Multiple Pulmonary Metastases from Lymphoma
- Renal Allograft Rejection (see Renal Allograft Rejection, [[Renal Allograft Rejection]])
- Abnormal vessel wall -> damage to RBC
- Mild thrombocytopenia
- Scleroderma (see Scleroderma, [[Scleroderma]])
- Mild thrombocytopenia
- Systemic Lupus Erythematosus* (see Systemic Lupus Erythematosus, [[Systemic Lupus Erythematosus]])
- Severe vasculitis -> fibrin deposition in vessels with damage to platelets and RBC
- Thrombocytopenia
- Thrombotic Thrombocytopenic Purpura (TTP) (see Thrombotic Thrombocytopenic Purpura, [[Thrombotic Thrombocytopenic Purpura]])
- Vasculitis (see Vasculitis, [[Vasculitis]])
- Infection
- Bartonellosis (see Bartonellosis, [[Bartonellosis]])
- Babesiosis (see Babesiosis, [[Babesiosis]])
- Clostridium Perfringens (see Clostridium Perfringens, [[Clostridium Perfringens]])
- E Coli (see E Coli, [[E Coli]])
- Leishmaniasis (see Leishmaniasis, [[Leishmaniasis]])
- Malaria (see Malaria, [[Malaria]])
- Pneumococcus (see Pneumococcus, [[Pneumococcus]])
- Staph Aureus (see Staph Aureus, [[Staph Aureus]])
- Other
- Near Drowning (see Near Drowning, [[Near Drowning]]): osmotic toxicity to RBC
- Severe Hypophosphatemia (see Hypophosphatemia, [[Hypophosphatemia]]): impaired RBC glycolysis with impaired ATP formation -> spherocyte formation
- Macroangiopathic Hemolytic Anemia
- Paroxysmal Nocturnal Hemoglobinuria (see Paroxysmal Nocturnal Hemoglobinuria, [[Paroxysmal Nocturnal Hemoglobinuria]])
- Physical Injury to RBC
- Heat
- Radiation
- Red Cell Membrane Defects
- Spur Cell Hemolysis
- Acquired Acanthocytosis
- Acquired Stomatocytosis
Acute Hemorrhage
- Gastrointestinal Bleed (see Gastrointestinal Bleed, [[Gastrointestinal Bleed]])
- Hemoperitoneum (see Hemoperitoneum, [[Hemoperitoneum]])
- Retroperitoneal Hemorrhage (see Retroperitoneal Hemorrhage, [[Retroperitoneal Hemorrhage]])
- Trauma: with external hemorrhage
Etiology of Relative Anemia (Increased Plasma Volume)
- Macroglobulinemia
- Pregnancy (see Pregnancy, [[Pregnancy]])
- Athletes
- Post-Flight Astronauts
Physiology
- Iron: free iron is toxic to cells and therefore, must be stored in alternate forms
- Within Cells: iron is complexed to protein, as ferritin or hemosiderin (apoferritin binds to free ferrous iron and stores it in its ferric state)
- As ferritin accumulates with cells of the reticuloendothelial system, protein aggregates are formed as hemosiderin -> hemosiderin is less readily available for utilization than ferritin is
- In the Circulation: serum iron is bound to transferrin
- Within Cells: iron is complexed to protein, as ferritin or hemosiderin (apoferritin binds to free ferrous iron and stores it in its ferric state)
- Predominant Site of Hemolysis
- Extravascular Hemolysis: RBC destruction in spleen and other reticuloendothelial tissues
- Autoimmune Hemolytic Anemia (AIHA): usually extravascular
- Hereditary Spherocytosis
- Intravascular Hemolysis: RBC destruction within vascular space
- Acute/Delayed Hemolytic Transfusion Reaction
- Autoimmune Hemolytic Anemia (AIHA): occurs in some cases where an antibody (usually IgM) forms an antibody-antigen complex on RBC membrane that is able to activate complement
- Favism
- Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency
- March Hemoglobinuria
- Microangiopathic Hemolytic Anemias (MAHA)
- Paroxysmal Cold Hemoglobinuria (PCH)
- Paroxysmal Nocturnal Hemoglobinuria (PNH)
- Sepsis
- Extravascular Hemolysis: RBC destruction in spleen and other reticuloendothelial tissues
Diagnosis
CBC
- MCV and MCH: usually increased in hemolysis (as retics are larger than mature RBC’s)
- Red Cell Distribution Width (RDW): reflects anisocytosis
Indirect Bilirubin
- Unconjugated bilirubinemia is seen in hemolysis (but is not specific, as it can also occur in Gilbert’s disease)
- In hemolysis, indirect bilirubin is usually <3 mg/dL (higher levels of indirect bilirubinemia indicate the presence of liver disease)
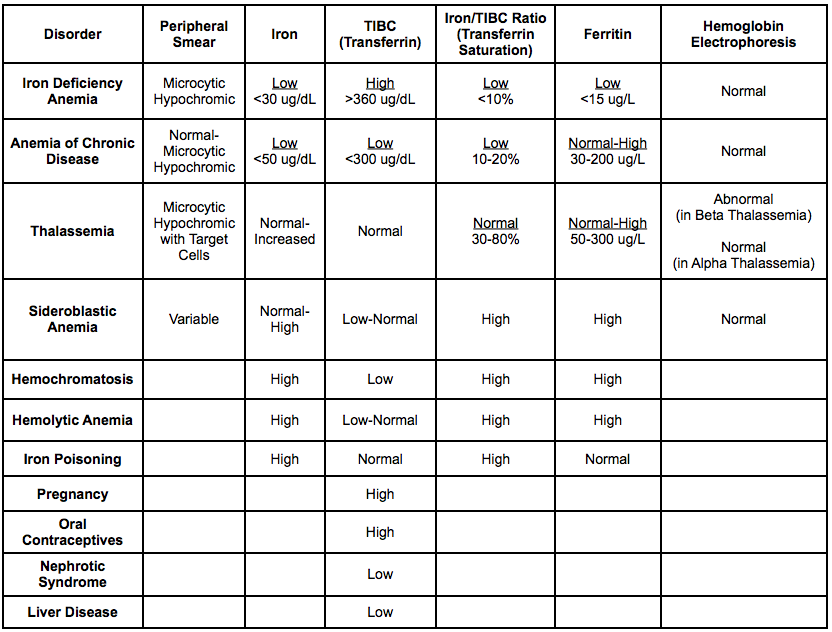
Iron Studies
- Iron: serum iron level represents the amount of circulating iron that is bound to transferrin (although this level varies diurnally)
- Normal: 50-150 ug/dL
- TIBC: indirect measure of the amount of circulating transferrin
- Normal: 300-360 ug/dL
- Transferrin Saturation (Iron/TIBC ratio x 100)
- Normal: 15-45%
- Level <15%: indicates iron deficiency
- Level 45-100%: indicates iron overload
- Ferritin: represents the total body iron store
- Normal (female): 20-200 ug/L -> average 100 ug/L
- Normal (male): 20-300 ug/L -> average 30 ug/L
- Level <12: indicates iron deficiency
- Level 300-4000: indicates iron overload
- Iron Studies in Various Disease States
Vitamin B12 Level
- Decreased in vitamin B12 deficiency
Folate Level
- Decreased in folate deficiency
LDH
- Increased in hemolysis (may be increased up to 10x normal with intravascular hemoylsis)
- Although LDH is sensitive for hemolysis, it is not specific (can be seen released from neoplastic cells, liver, lung, etc)
Haptoglobin
- Decreased in hemolysis (decrease in haptoglobin is more likely in intravascular hemolysis than in extravascular hemolysis)
- However, haptoglobin is an acute phase reactant -> can increase in infections and in other reactive states
Urine Hemoglobin
- Hemoglobinuria (“Coca Cola”-colored urine): increased in intravascular hemolysis
- Hemosiderinuria: presence suggests severe or intravascular hemolysis
- Hemosiderin can be detected in iron-stained urinary sediment (within sloughed renal epithelial cells)
- With severe and intravascular hemolysis, urinary hemoglobin is reabsorbed by renal tubular cells and processed to hemosiderin
Urobilinogen
- Increased in urine and stool in hemolysis
Peripheral Smear
- Hypochromia : enlarged area of central pallor
- Etiology
- Iron Deficiency Anemia (see Iron Deficiency Anemia, [[Iron Deficiency Anemia]])
- Etiology
- Pencil Cells: elongated pencil-shaped RBC’s
- Etiology
- Iron Deficiency Anemia (see Iron Deficiency Anemia, [[Iron Deficiency Anemia]])
- Etiology
- Schistocytes: fragmented RBC’s
- Etiology
- Thrombotic Thrombocytopenic Purpura (TTP)/Hemolytic Uremic Syndrome (HUS)
- Mechanical RBC Damage
- Etiology
- Target Cells
- Spur Cells
- Etiology
- Spur Cell Anemia
- Etiology
- Leukoerythroblastic Smear: smear with precursor cells of the myeloid and erythroid lineage, which usually indicates the presence of extramedullary hematopoiesis (predominantly in the spleen)
- Etiology
- Bone Marrow Infiltration (see Pancytopenia, [[Pancytopenia]])
- Myelofibrosis/Myelophthisis (see Pancytopenia, [[Pancytopenia]])
- Severe Stress: due to blood loss, infection, hemolysis, etc
- Features
- Immature Myeloid Cells
- Megakaryocytic Fragments
- Teardrop-Shaped RBC (Dacrocytes)
- Immature Nucleated RBC
- Anisocytosis:
- Poikilocytosis
- Polychromasia: indicates RBC immaturity
- Etiology
- Spherocytes
- Etiology
- Hereditary Spherocytosis
- Hypophosphatemia (see Hypophosphatemia, [[Hypophosphatemia]]): severe
- Autoimmune Hemolytic Anemia (AIHA)
- Etiology
Reticulocytes
- Reticulocytes are newly-released RBC’s: they are slightly larger than mature RBC’s and have some residual ribosomal RNA -> presence of RNA allows for staining, with detection and counting)
- Retic Index = Retic Count x (Patient’s Hct/Normal Hct)
- Use Normal Hct = 45%
- Retic Index > or = to 2.5 -> indicates hemolysis or subacute hemorrhage (acute hemorrhage may not result in an increased retic index, because of the time that it takes to increase epo synthesis and increase marrow RBC production)
- Retic Index <2.5 -> indicates chronic anemia, hypoproliferative anemia (iron deficiency, marrow hyporesponsiveness, aplasia) or a maturation disorder (vitmain B2 deficiency, etc)
Direct Coombs Test (Direct Anti-Globulin Test)
- Usually Positive in Immune Hemolytic Anemias: however, about 5-10% of autoimmune hemolytic anemia cases are direct Coombs-negative
- Polybrene Test: can be used to diagnose direct Coombs-negative autoimmune hemolytic anemia
Clinical Differentiation of Hemolytic Syndromes

Clinical Differentiation of Intravascular Hemolysis Syndromes

Clinical Manifestations
Cardiovascular Manifestations
Angina/Chest Pain (see Chest Pain, [[Chest Pain]])
- xxxx
Dermatologic Manifestations
Pallor
- xxxx
Pulmonary Manifestations
Dyspnea (see Dyspnea, [[Dyspnea]])
- xxxx
Other Manifestations
- xxxx
Treatment
Iron
- Agents
- Ferrous Sulfate (see Ferrous Sulfate, [[Ferrous Sulfate]])
- Clinical Efficacy
- Systematic Review and Meta-Analysis of Intravenous Iron in Decreasing the Need for Allogenic Packed Red Blood Cell Transfusion (BMJ, 2013) [MEDLINE]
- Intravenous Iron is Effective in Increasing Hemoglobin Concentration and Decreasing the Risk of Allogeneic Packed Red Blood Cell Transfusion
- Intravenous Iron Increased the Risk of Infection, as Compared to Oral Iron or No Iron Supplementation
- Systematic Review and Meta-Analysis of Intravenous Iron in Decreasing the Need for Allogenic Packed Red Blood Cell Transfusion (BMJ, 2013) [MEDLINE]
Erythropoetin (see Erythropoetin, [[Erythropoetin]])
- Clinical Efficacy
- EPO Critical Care Trials Group Study (NEJM, 2006) [MEDLINE]
- Use of epoetin alfa does not reduce the incidence of red-cell transfusion among critically ill patients, but it may reduce mortality in patients with trauma
- Treatment with epoetin alfa is associated with an increase in the incidence of thrombotic events
- EPO Critical Care Trials Group Study (NEJM, 2006) [MEDLINE]
Packed Red Blood Cells (PRBC) (see Packed Red Blood Cells, [[Packed Red Blood Cells]])
- Clinical Efficacy in Cardiac Surgery Patients
- TRACS Trial in Cardiac Surgery Patients (JAMA, 2010) [MEDLINE]
- Restrictive Transfusion Strategy (Maintenance of Hct >24%) was Non-Inferior to a Liberal Transfusion Strategy (Maintenance of Hct >30%) with Regard to 30-Day All-Cause Mortality and Other Severe Morbities
- Regardless of the Transfusion Strategy, an Increased Number of Transfusions was Associated with Increased Clinical Complications and Increased 30-Day Mortality
- TRACS Trial in Cardiac Surgery Patients (JAMA, 2010) [MEDLINE]
- Clinical Efficacy in General Intensive Care Unit/Sepsis Patients
- Canadian Critical Care Trials Group Transfusion Requirements in Critical Care (TRICC) Trial (NEJM, 1999) [MEDLINE]: trial comparing transfusion cut-offs of Hb 7g/dL vs 10 g/dL (trial excluded: acute myocardial infarction and unstable angina)
- No Overall Difference in 30-Day Mortality: however, less acutely ill (APACHE score of ≤20) and <55 y/o groups had lower mortality rates with the restrictive transfusion strategy
- Restrictive Transfusion Strategy Decreased Hospital Mortality Rate
- Transfusion Requirements in Septic Shock (TRISS) Trial (NEJM, 2014) [MEDLINE]: Danish multi-center RCT (n = 998) comparing hemoglobin of 7 g/dL vs 9 g/dL in septic shock (trial excluded: acute myocardial ischemia, acute burn injury, previous PRBC transfusion, and acute life-threatening bleeding) -> primary outcome: 90-day mortality
- No Difference in Mortality (and Rates of Ischemic Events, Transfusion Reactions, and Use of Life Support) Between the Groups: however, the 7 g/dL group had lower PRBC utilization
- Canadian Critical Care Trials Group Transfusion Requirements in Critical Care (TRICC) Trial (NEJM, 1999) [MEDLINE]: trial comparing transfusion cut-offs of Hb 7g/dL vs 10 g/dL (trial excluded: acute myocardial infarction and unstable angina)
- Clinical Efficacy in Critical Care Patients
- Recommendations
- Transfusion Threshold of Hb 7 g/dL Appears to Be Appropriate
- Choosing Wisely Campaign Recommends to Not Transfuse PRBC’s in Non-Bleeding ICU Patients with Hb >7 g/dL (Am J Resp Crit Care Med, 2014) [MEDLINE]
References
- A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999;340:409-417 [MEDLINE]
- Diagnosis and management of iron-related anemias in critical illness. Crit Care Med 2006; 34:1898 -1905
- Managing anemia in critically ill adults. Br Med J 2010; 341:c4408
- Efficacy and safety of epoetin alfa in critically ill patients. N Engl J Med 2007; 357:965-976 [MEDLINE]
- Transfusion requirements after cardiac surgery. The TRACS randomized controlled trial. JAMA 2010; 304:1559-1567 [MEDLINE]
- Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomised clinical trials. BMJ. 2013 Aug 15;347:f4822. doi: 10.1136/bmj.f4822 [MEDLINE]
- An official American Thoracic Society/American Association of Critical-Care Nurses/American College of Chest Physicians/Society of Critical Care Medicine policy statement: the Choosing Wisely® Top 5 list in Critical Care Medicine. Am J Respir Crit Care Med. 2014 Oct 1;190(7):818-26. doi: 10.1164/rccm.201407-1317ST [MEDLINE]
- Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2014 Oct 9;371(15):1381-91. doi: 10.1056/NEJMoa1406617. Epub 2014 Oct 1 [MEDLINE]
