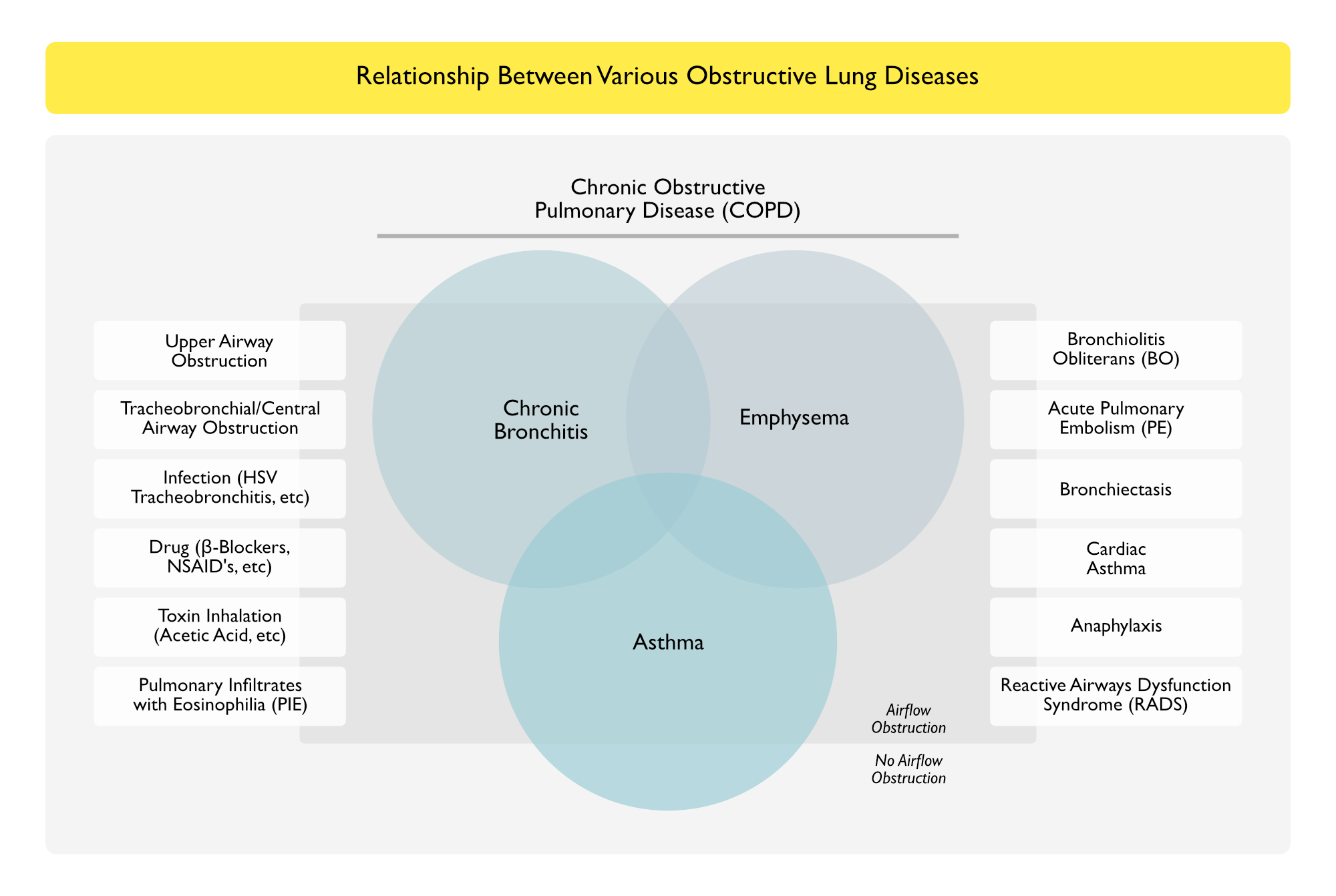
Relationship Between Various Obstructive Lung Diseases
- Key Points
- Classical Obstructive Lung Diseases, Such as Chronic Obstructive Pulmonary Disease and Asthma, May or May Not Demonstrate Obstruction
- Obstruction (with Wheezing, etc) Can Also Be Variably Present in Other Airway and Lung Diseases

Upper Airway Obstruction
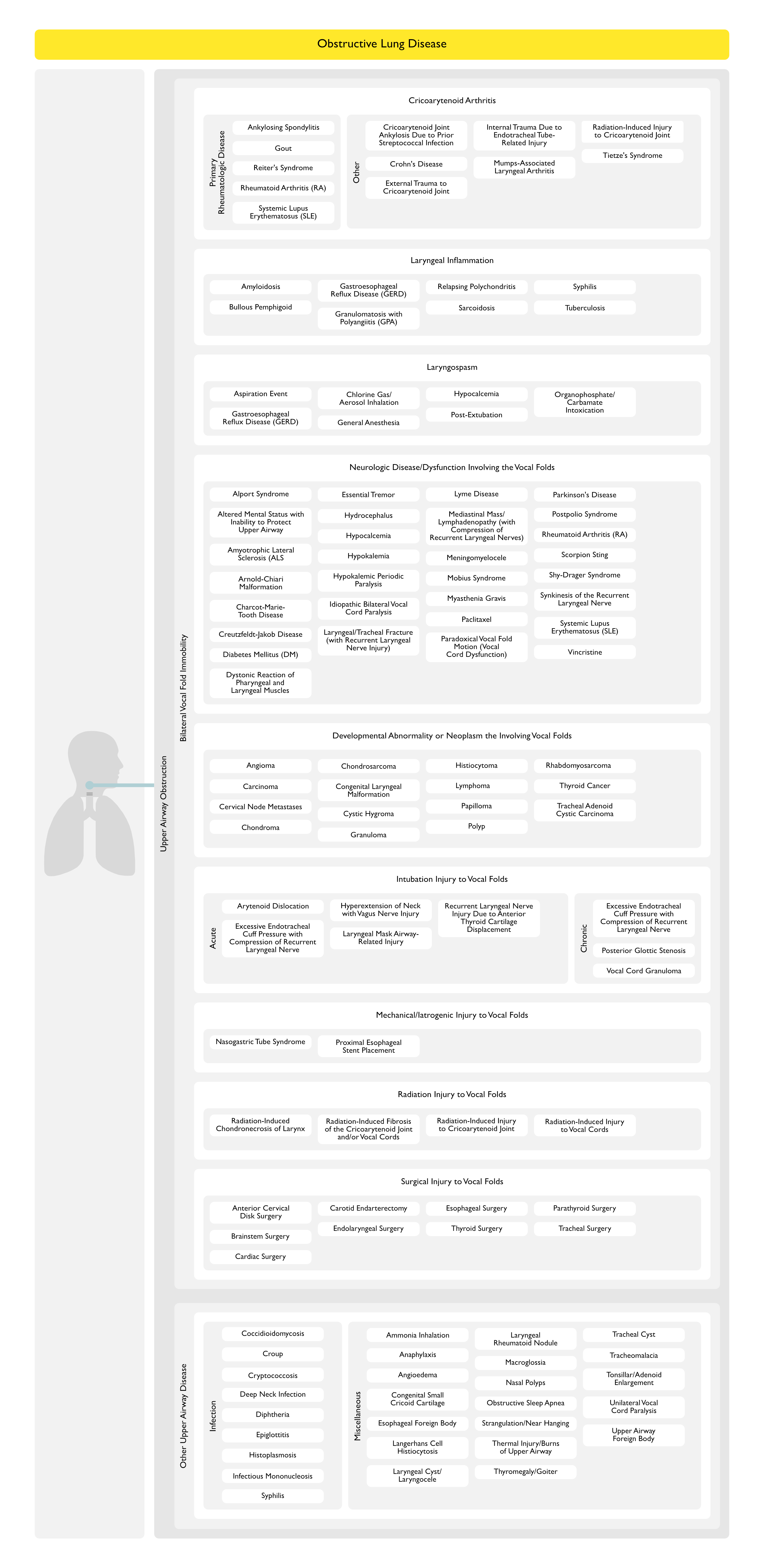
Bilateral Vocal Fold Immobility (BVFI) (see Bilateral Vocal Fold Immobility)
Cricoarytenoid Arthritis (see Cricoarytenoid Arthritis)
- Primary Rheumatologic Disease
- Ankylosing Spondylitis (see Ankylosing Spondylitis)
- Gout (see Gout)
- Reiter’s Syndrome (see Reiter’s Syndrome)
- Rheumatoid Arthritis (RA) (see Rheumatoid Arthritis)
- Rheumatoid Nodules May Occur in the Soft Tissues Surrounding the Cricoarytenoid Joint
- Systemic Lupus Erythematosus (SLE) (see Systemic Lupus Erythematosus)
- Other
- Cricoarytenoid Joint Ankylosis Due to Prior Streptococcal Infection (see Streptococcus)
- Crohn’s Disease (see Crohn’s Disease)
- External Trauma to Cricoarytenoid Joint
- Internal Trauma Due to Endotracheal Tube-Related Injury to the Cricoarytenoid Joint
- Manifestations
- Anterior or Posterior Arytenoid Displacement
- Posterior Dislocation Resulting from Extubation with a Partially Inflated Endotracheal Tube Cuff
- Arytenoid Chondritis Secondary to Prolonged Endotracheal Intubation
- Manifestations
- Mumps-Associated Laryngeal Arthritis (see Mumps Virus)
- Radiation Therapy Injury to Cricoarytenoid Joint (see Radiation Therapy)
- Tietze’s Syndrome (see Tietze’s Syndrome)
Laryngeal Inflammation
- Amyloidosis (see Amyloidosis)
- Bullous Pemphigoid of Upper Airway (see Bullous Pemphigoid)
- Gastroesophageal Reflux Disease (GERD) (see Gastroesophageal Reflux Disease)
- Granulomatosis with Polyangiitis (GPA) (Wegener’s Granulomatosis) (see Granulomatosis with Polyangiitis)
- Relapsing Polychondritis (see Relapsing Polychondritis)
- Sarcoidosis (see Sarcoidosis)
- Syphilis (see Syphilis)
- Clinical
- May Be Acute or Progressive
- Clinical
- Tuberculosis (see Tuberculosis)
Laryngospasm (see Laryngospasm)
- Aspiration Event (see Aspiration Pneumonia)
- Epidemiology
- Associated with Intubation for Mechanical Ventilation (see Invasive Mechanical Ventilation-General)
- Associated with Procedural Sedation (see Sedation)
- Epidemiology
- Gastroesophageal Reflux Disease (GERD) (see Gastroesophageal Reflux Disease)
- Chlorine Gas/Aerosol Inhalation (see Chlorine)
- General Anesthesia (see General Anesthesia)
- Epidemiology
- Laryngospasm Typically Occurs on Emergence from General Anesthesia
- Epidemiology
- Hypocalcemia (see Hypocalcemia)
- Post-Extubation
- Organophosphate Intoxication (see Organophosphates-Carbamates)
- Physiology
- Nicotinic Effects Cause Laryngospasm
- Physiology
Neurologic Disease/Dysfunction Involving the Vocal Folds
- Alport Syndrome (see Alport Syndrome)
- Epidemiology
- Case Report Involved a Patient with Chronic Kidney Disease, Postoperative from Surgery with Large Amount of Blood Loss and Possible Impaired Perfusion to Recurrent Laryngeal Nerves (with Ischemic Injury) During the Case
- Epidemiology
- Altered Mental Status with Inability to Protect Upper Airway
- Amyotrophic Lateral Sclerosis (ALS) (see Amyotrophic Lateral Sclerosis)
- Arnold-Chiari Malformation
- Charcot-Marie-Tooth Disease
- Creutzfeldt-Jakob Disease (CJD) (see Creutzfeldt-Jakob Disease)
- Diabetes Mellitus (DM) (see Diabetes Mellitus)
- Physiology
- Neuropathy Involving the Laryngeal Nerves
- Physiology
- Dystonic Reaction of Pharyngeal and Laryngeal Muscles (see Dystonic Reaction of Pharyngeal+Laryngeal Muscles): typically acute
- Essential Tremor (see Essential Tremor)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Hydrocephalus (see Hydrocephalus)
- Hypocalcemia (see Hypocalcemia)
- Hypokalemia (see Hypokalemia)
- Hypokalemic Periodic Paralysis (see Hypokalemic Periodic Paralysis)
- Idiopathic Bilateral Vocal Cord Paralysis
- Laryngeal/Tracheal Fracture (with Recurrent Laryngeal Nerve Injury) (see Tracheobronchial Fracture)
- Lyme Disease (see Lyme Disease)
- Physiology
- Neuropathy Involving the Laryngeal Nerves
- Physiology
- Mediastinal Mass/Lymphadenopathy (with Compression of Recurrent Laryngeal Nerves)see Mediastinal Mass)
- Meningomyelocele
- Mobius Syndrome
- Myasthenia Gravis (see Myasthenia Gravis)
- Paclitaxel (Taxol) (see Paclitaxel)
- Physiology
- Neuropathy Involving the Laryngeal Nerves
- Physiology
- Paradoxical Vocal Fold Motion (Vocal Cord Dysfunction) (see Paradoxical Vocal Fold Motion)
- Clinical
- Typically acute
- Clinical
- Parkinson’s Disease (see Parkinson’s Disease)
- Clinical
- May Be Acute (Particularly in the Postoperative Setting) or Progressive
- Clinical
- Postpolio Syndrome (see Poliomyelitis)
- Rheumatoid Arthritis (RA) (see Rheumatoid Arthritis)
- Physiology
- Arteritis of Vasa Vasorum of Recurrent Laryngeal/Vagus Nerves
- Physiology
- Shy-Drager Syndrome
- Synkinesis of the Recurrent Laryngeal Nerve
- Systemic Lupus Erythematosus (SLE) (see Systemic Lupus Erythematosus)
- Physiology
- Neuropathy Involving the Laryngeal Nerves
- Physiology
- Vincristine (see Vincristine)
- Physiology
- Neuropathy Involving the Laryngeal Nerves
- Physiology
Developmental Abnormality or Neoplasm the Involving Vocal Folds
- Angioma
- Carcinoma
- Cervical Node Metastases (with Extrinsic Compression of Upper Airway)
- Thyroid Cancer (see Thyroid Cancer)
- Head and Neck Cancer (Squamous Cell Carcinoma (see Head and Neck Cancer)
- Chondroma
- Chondrosarcoma
- Congenital Laryngeal Malformation
- Cystic Hygroma
- Granuloma
- Histiocytoma
- Lymphoma (see Lymphoma)
- Papilloma
- Polyp
- Rhabdomyosarcoma (see Rhabdomyosarcoma)
- Thyroid Cancer (see Thyroid Cancer)
- Tracheal Adenoid Cystic Carcinoma (see Adenoid Cystic Carcinoma)
Intubation Injury to Vocal Folds (see Endotracheal Tube-Associated Laryngeal Injury)
- Acute
- Arytenoid Dislocation
- Excessive Endotracheal Cuff Pressure with Compression of Recurrent Laryngeal Nerve Where It Enters the Larynx
- Hyperextension of Neck with Vagus Nerve Injury
- Larygneal Mask Airway (LMA)-Related Injury
- Recurrent Laryngeal Nerve Injury Due to Anterior Thyroid Cartilage Displacement (Relative to the Cricoid Cartilage)
- Chronic
- Excessive Endotracheal Tube Cuff Pressure with Compression of Recurrent Laryngeal Nerve Where It Enters the Larynx
- Posterior Glottic Stenosis (PGS): due to prolonged or traumatic intubation
- Vocal Cord Granuloma
Mechanical/Iatrogenic Injury to Vocal Folds
- Nasogastric Tube Syndrome (see Nasogastric Tube Syndrome)
- Epidemiology
- First Reported in 1981
- Risk Group
- Diabetic Renal Transplant Patients (Due to Prolonged Gastroparesis and Requirement for Nasogastric Tube Drainage)
- Epidemiology
- Proximal Esophageal Stent Placement (see Esophageal Stent)
Radiation Injury to Vocal Folds (see Radiation Therapy)
- Radiation-Induced Chondronecrosis of Larynx
- Radiation-Induced Fibrosis of the Cricoarytenoid Joint and/or Vocal Cords
- Radiation-Induced Injury to Cricoarytenoid Joint: see Cricoarytenoid Arthritis above
- Radiation Injury to Vocal Cords
Surgical Injury to Vocal Folds
- Anterior Cervical Disk Surgery
- Epidemiology
- Typically Results in Unilateral Injury (Which May Compromise the Upper Airway if Contralateral Side was Previously Injured)
- Epidemiology
- Brainstem Surgery
- Epidemiology
- May Result in Bilateral Injury
- Epidemiology
- Cardiac Surgery
- Carotid Endarterectomy
- Epidemiology
- Typically Results in Unilateral Injury (Which May Compromise the Upper Airway if Contralateral Side was Previously Injured)
- Epidemiology
- Endolaryngeal Surgery (Using Carbon Dioxide Laser)
- Epidemiology
- May Damage the Posterior Glottis
- Epidemiology
- Esophageal Surgery
- Epidemiology
- May Result in Bilateral Injury
- Epidemiology
- Thyroid Surgery
- Epidemiology
- Accounts for 48% of All Surgical Cases
- May Result in Bilateral Injury
- Epidemiology
- Parathyroid Surgery
- Epidemiology
- May Result in Bilateral Injury
- Epidemiology
- Tracheal Surgery
- Epidemiology
- May Result in Bilateral Injury
- Epidemiology
Other Upper Airway Disease
Infection
- Coccidioidomycosis (see Coccidioidomycosis)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Croup (see Croup)
- Clinical
- Typically Acute
- Clinical
- Cryptococcosis (see Cryptococcosis)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Deep Neck Infection (see Deep Neck Infection)
- General Comments
- Typically Acute
- Peritonsillar Abscess (Involving Peritonsillar Space) (see Peritonsillar Abscess)
- Pretracheal Abscess (Involving Pretracheal Space) (see Pretracheal Abscess)
- Retropharyngeal Abscess (Involving Retropharyngeal Space) (see Retropharyngeal Abscess)
- Submandibular Space Abscess/Ludwig’s Angina (Involving Submandibular Space) (see Ludwig’s Angina)
- General Comments
- Diphtheria (see Diphtheria)
- Clinical
- Typically Acute
- Clinical
- Epiglottitis (see Epiglottitis)
- Clinical
- Typically Acute
- Clinical
- Histoplasmosis (see Histoplasmosis)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Syphilis (see Syphilis)
Miscellaneous
- Ammonia Inhalation (see Ammonia)
- Clinical
- Typically Acute
- Clinical
- Anaphylaxis (see Anaphylaxis)
- Clinical
- Typically Acute
- Clinical
- Angioedema (see Angioedema)
- Clinical
- Typically Acute
- Clinical
- Congenital Small Cricoid Cartilage
- Clinical
- Typically Progressive
- Clinical
- Esophageal Foreign Body
- Physiology
- Extrinsic Compression of Upper Airway
- Clinical
- Typically Progressive
- Physiology
- Langerhans Cell Histiocytosis (see Langerhans Cell Histiocytosis)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Laryngeal Cyst/Laryngocele
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Laryngeal Rheumatoid Nodule (see Rheumatoid Arthritis)
- Clinical
- Typically Progressive
- Clinical
- Macroglossia
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Nasal Polyps (see Nasal Polyps)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Obstructive Sleep Apnea (OSA) (see Obstructive Sleep Apnea)
- Epidemiology
- More Commonly Occurs in the Postoperative Setting*
- Clinical
- Typically Acute
- Epidemiology
- Strangulation/Near Hanging (see Near Hanging)
- Epidemiology
- In Non-Judicial Hangings (Where he Drop is <6.5-7.5 ft) and the Dens Does Not Fracture Off, Death Most Commonly Occurs Due to Pulmonary Complications
- Epidemiology
- Thermal Injury/Burns of Upper Airway (see Smoke Inhalation)
- Clinical
- May Be Acute
- Thermal injury is usually supraglottic (typically, laryngeal injury)
- Clinical
- Thyromegaly/Goiter (see Goiter)
- Clinical
- Typically Progressive
- Clinical
- Tracheal Cyst
- Clinical
- Typically Progressive
- Clinical
- Tracheomalacia (see Tracheobronchomalacia)
- Clinical
- Typically Progressive
- Clinical
- Tonsillar/Adenoid Enlargement
- Clinical
- Typically Progressive
- Clinical
- Unilateral Vocal Cord Paralysis (see Unilateral Vocal Fold Immobility)
- Clinical
- Typically Mild Upper Airway Obstruction
- Clinical
- Upper Airway Foreign Body (see Airway Foreign Body)
- Clinical
- Typically Acute
- Clinical
Tracheobronchial/Central Airway Obstruction (see Central Airway Obstruction)
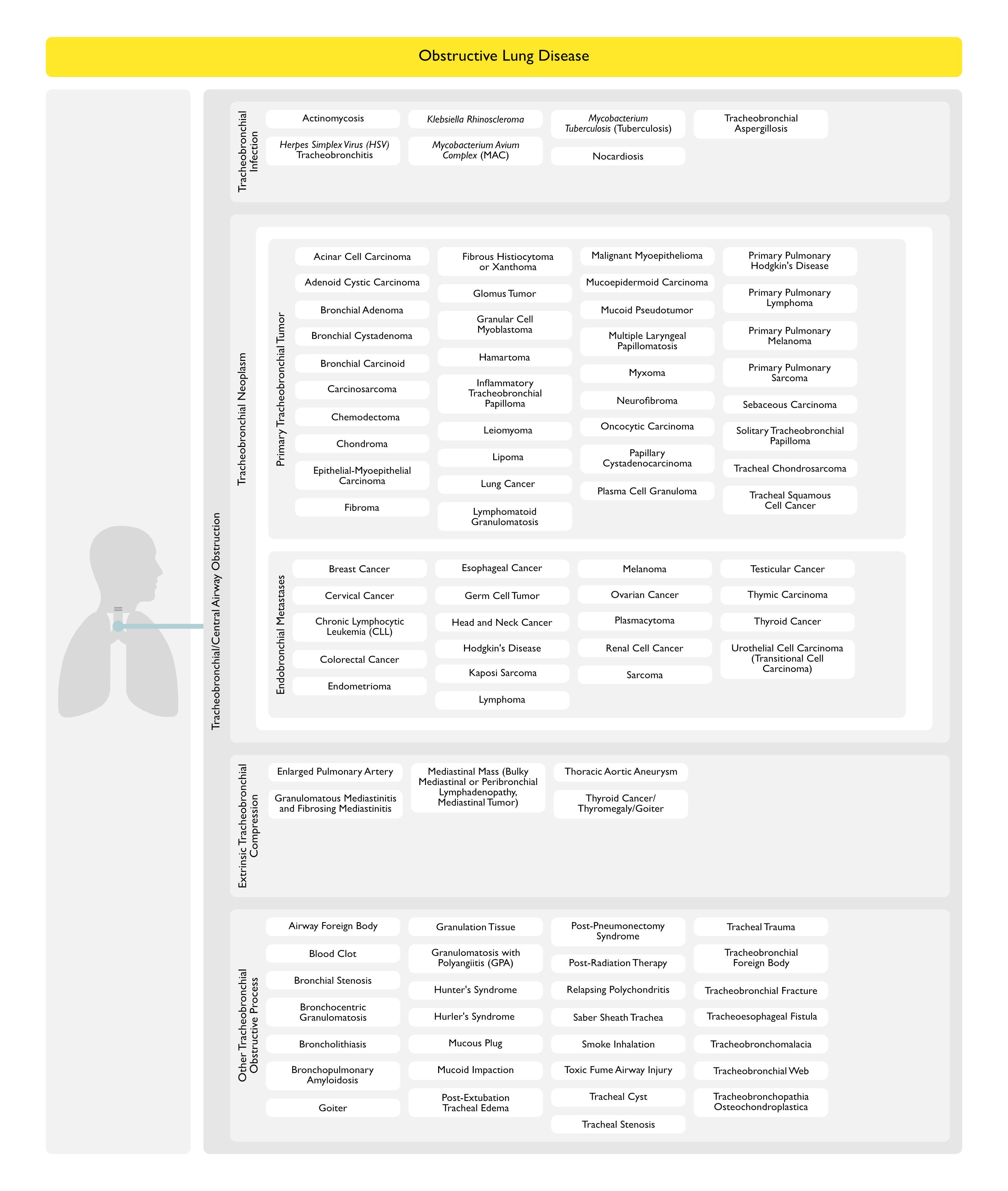
Tracheobronchial Infection
- Herpes Simplex Virus (HSV) Tracheobronchitis (see Herpes Simplex Virus)
- Klebsiella Rhinoscleroma (see Klebsiella Rhinoscleroma)
- Mycobacterium Avium Complex (MAC) (see Mycobacterium Avium Complex)
- Tracheobronchial Aspergillosis (see Tracheobronchial Aspergillosis)
- Tuberculosis (see Tuberculosis)
Tracheobronchial Neoplasm
Primary Tracheobronchial Tumor
- Acinar Cell Carcinoma (see Acinar Cell Carcinoma)
- Adenoid Cystic Carcinoma (see Adenoid Cystic Carcinoma)
- Bronchial Adenoma (see Bronchial Adenoma)
- Bronchial Cystadenoma (see Bronchial Cystadenoma)
- Bronchial Carcinoid (see Bronchial Carcinoid)
- Carcinosarcoma (see Carcinosarcoma)
- Chemodectoma (see Chemodectoma)
- Chondroma (see Chondroma)
- Epithelial-Myoepithelial Carcinoma (see Epithelial-Myoepithelial Carcinoma)
- Fibroma (see Fibroma)
- Fibrous Histiocytoma or Xanthoma (see Fibrous Histiocytoma or Xanthoma)
- Glomus Tumor(see Glomus Tumor)
- Granular Cell Myoblastoma (see Granular Cell Myoblastoma)
- Hamartoma (see Hamartoma)
- Inflammatory Tracheobronchial Papilloma (see Inflammatory Tracheobronchial Papilloma)
- Leiomyoma (see Leiomyoma)
- Lipoma (see Lipoma)
- Lung Cancer (see Lung Cancer): common etiology
- Lymphomatoid Granulomatosis (see Lymphomatoid Granulomatosis)
- Malignant Myoepithelioma (see Malignant Myoepithelioma)
- Mucoepidermoid Carcinoma (see Mucoepidermoid Carcinoma)
- Mucoid Pseudotumor (see Mucoid Pseudotumor)
- Multiple Laryngeal Papillomatosis (see Multiple Laryngeal Papillomatosis)
- Myxoma (see Myxoma)
- Neurofibroma (see Neurofibroma)
- Oncocytic Carcinoma
- Papillary Cystadenocarcinoma
- Plasma Cell Granuloma (see Plasma Cell Granuloma)
- Primary Pulmonary Hodgkin’s Disease (see Primary Pulmonary Hodgkins Disease)
- Primary Pulmonary Lymphoma (see Primary Pulmonary Lymphoma)
- Primary Pulmonary Melanoma (see Primary Pulmonary Melanoma)
- Primary Pulmonary Sarcoma (see Primary Pulmonary Sarcoma)
- Sebaceous Carcinoma (see Sebaceous Carcinoma)
- Solitary Tracheobronchial Papilloma (see Solitary Tracheobronchial Papilloma)
- Tracheal Chondrosarcoma (see Chondrosarcoma)
- Tracheal Squamous Cell Cancer (see Tracheal Squamous Cell Cancer)
Endobronchial Metastases (see also Lung Metastases-Endobronchial)
- Breast Cancer (see Breast Cancer)
- Cervical Cancer (see Cervical Cancer)
- Chronic Lymphocytic Leukemia (CLL) (see Chronic Lymphocytic Leukemia)
- Colorectal Cancer (see Colorectal Cancer)
- Endometrioma (see Endometrioma)
- Esophageal Cancer (see Esophageal Cancer)
- Germ Cell Tumor (see Germ Cell Tumor)
- Head and Neck Cancer (see Head and Neck Cancer)
- Hodgkin’s Disease (see Hodgkins Disease)
- Kaposi Sarcoma (see Kaposi Sarcoma)
- Lymphoma (see Lymphoma)
- Melanoma (see Melanoma)
- Ovarian Cancer (see Ovarian Cancer)
- Plasmacytoma (see Multiple Myeloma])
- Renal Cell Cancer (see Renal Cancer)
- Sarcoma
- Testicular Cancer (see Testicular Cancer)
- Thymic Carcinoma (see Thymoma)
- Thyroid Cancer (see Thyroid Cancer)
- Urothelial Cell Carcinoma (Transitional Cell Carcinoma) (see Urothelial Cell Carcinoma)
- Bladder Cancer (see Bladder Cancer)
- Renal Cancer (see Renal Cancer)
- Ureteral Cancer (see Ureteral Cancer)
- Urethral Cancer (see Urethral Cancer])
Extrinsic Tracheobronchial Compression
- Enlarged Pulmonary Artery: extrinsic compression of tracheobronchial airways
- Tetralogy of Fallot (see Tetralogy of Fallot): in infants and children
- Transposition of Great Vessles with Ventricular Septal Defect: in infants and children
- Granulomatous Mediastinitis and Fibrosing Mediastinitis (see Granulomatous Mediastinitis and Fibrosing Mediastinitis])
- Physiology: extrinsic compression of tracheobronchial airways
- Mediastinal Mass (see Mediastinal Mass): extrinsic compression of tracheobronchial airways
- Bulky Mediastinal or Peribronchial Lymphadenopathy
- Cancer
- Hodgkin’s Disease (see Hodgkin’s Disease)
- Lymphoma (see Lymphoma)
- Tuberculosis (see Tuberculosis): involvement of mediastinal nodes may compress RML bronchus
- Sarcoidosis (see Sarcoidosis)
- Mediastinal Tumor
- Bulky Mediastinal or Peribronchial Lymphadenopathy
- Thoracic Aortic Aneurysm (TAA) (see Thoracic Aortic Aneurysm): extrinsic compression of tracheobronchial airways
- Thyroid Cancer/Thyromegaly/Goiter (see Goiter and Thyroid Cancer)
- Physiology: extrinsic compression of trachea
Other Tracheobronchial Obstructive Process
- Airway Foreign Body (see Airway Foreign Body)
- Blood Clot
- Epidemiology
- Airway Obstruction by Blood Clots Typically Occurs Following Significant Hemoptysis
- Epidemiology
- Bronchial Stenosis (see Bronchial Stenosis)
- Bronchocentric Granulomatosis (see Bronchocentric Granulomatosis)
- Broncholithiasis (see Broncholithiasis)
- Bronchopulmonary Amyloidosis (see Amyloidosis)
- Goiter
- Granulation Tissue
- Airway Foreign Body
- Airway Stent
- Endotracheal Tube
- Surgical Airway Anastomosis (see Lung Transplant)
- Tracheostomy Tube (see Tracheostomy)
- Granulomatosis with Polyangiitis (Wegener’s Granulomatosis) (see Granulomatosis with Polyangiitis)
- Hunter’s Syndrome
- Physiology
- Due to Tracheal Stenosis
- Physiology
- Hurler’s Syndrome
- Physiology
- Due to Tracheal Stenosis
- Physiology
- Mucous Plug (see Mucous Plug)
- Epidemiology
- Tracheobronchial Obstruction by Mucous Plugging is Common in Patients with Lung Disease and Infection in the Intensive Care Unit Setting
- Epidemiology
- Mucoid Impaction (see Mucoid Impaction)
- Physiology
- Tracheobronchial Obstruction
- Physiology
- Post-Extubation Tracheal Edema
- Post-Pneumonectomy Syndrome (see Post-Pneumonectomy Syndrome)
- Post-Radiation Therapy (see Radiation Therapy)
- Physiology
- Bronchial Granulation Tissue (or Stricture)
- Physiology
- Relapsing Polychondritis (see Relapsing Polychondritis)
- Physiology
- Endotracheal or Endobronchial Obstruction by Loss of Supporting Cartilage in Airways
- Physiology
- Saber Sheath Trachea (see Saber Sheath Trachea)
- Smoke Inhalation (see Smoke Inhalation)
- Physiology
- Tracheobronchial Mucosal Injury with Sloughing and Airway Obstruction
- Physiology
- Toxic Fume Airway Injury
- Physiology
- Tracheobronchial Mucosal Injury with Sloughing and Airway Obstruction
- Physiology
- Tracheal Cyst (see Tracheal Cyst)
- Tracheal Stenosis (see Tracheal Stenosis)
- Tracheal Trauma
- Tracheobronchial Foreign Body (see Airway Foreign Body)
- Tracheobronchial Fracture (see Tracheobronchial Fracture)
- Tracheoesophageal Fistula (see Tracheoesophageal Fistula)
- Tracheobronchomalacia (see Tracheobronchomalacia)
- Tracheobronchial Web
- Epidemiology
- Idiopathic
- Sarcoidosis (see Sarcoidosis)
- Tuberculosis (see Tuberculosis)
- Epidemiology
- Tracheobronchopathia Osteochondroplastica (see Tracheobronchopathia Osteochondroplastica)
Other Airway Obstruction
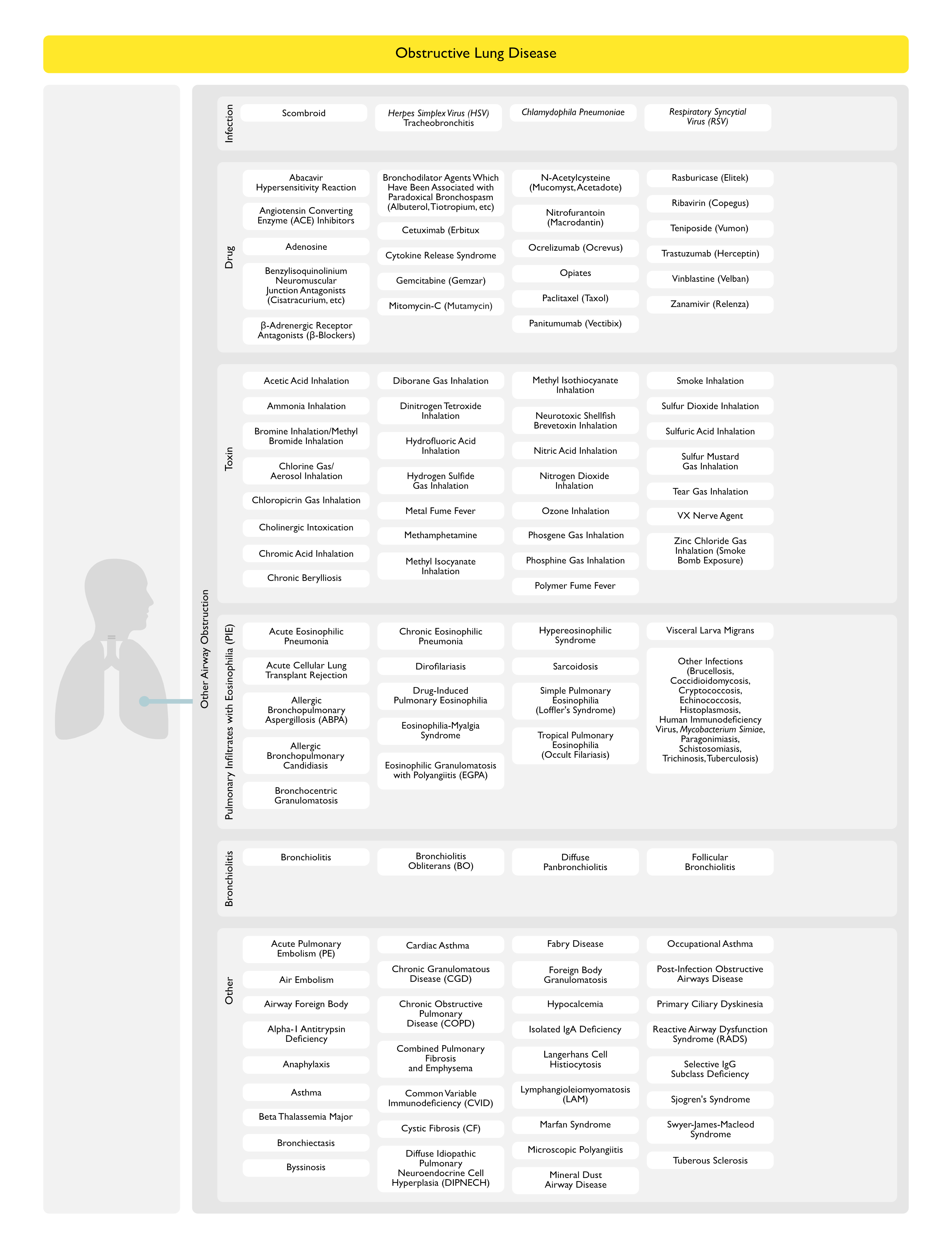
Infection
- Scombroid (see Scombroid)
- Physiology
- Ingestion of Histamine-Contaminated Fish (or Swiss Cheese)
- Clinical
- Bronchospasm (Cough, Dyspnea, Wheezing) May Be Severe in Patients with Underlying Lung Disease
- Physiology
- Herpes Simplex Virus (HSV) Tracheobronchitis (see Herpes Simplex Virus)
- Chlamydophila Pneumoniae (see Chlamydophila Pneumoniae)
Drug
- Abacavir Hypersensitivity Reaction (see Abacavir)
- Angiotensin Converting Enzyme (ACE) Inhibitors (see Angiotensin Converting Enzyme Inhibitors)
- Epidemiology
- Rarely, May Exacerbate Bronchospasm
- Epidemiology
- Adenosine (see Adenosine)
- Epidemiology
- May Cause Brief Bronchospasm When Used in the Diagnosis of Arrhythmias
- Epidemiology
- Benzylisoquinolinium Neuromuscular Junction Antagonists (see Neuromuscular Junction Antagonists)
- Agents
- Alcuronium
- Atracurium (Tracrium) (see Atracurium)
- Cisatracurium (Nimbex) (see Cisatracurium)
- Doxacurium (see Doxacurium)
- Mivacurium (see Mivacurium)
- Tubocurarine
- Pharmacology
- Histamine Release-Mediated Bronchospasm
- Agents
- β-Adrenergic Receptor Antagonists (Beta Blockers) (see β-Adrenergic Receptor Antagonists)
- Bronchodilator Agents Which Have Been Associated with Paradoxical Bronchospasm
- Agents
- Aclidinium (Tudorza Pressair) (see Aclidinium)
- Albuterol (Ventolin) (see Albuterol)
- Tiotropium (Spiriva) (see Tiotropium)
- Tiotropium + Olodaterol (Stiolto Respimat) (see Tiotropium + Olodaterol)
- Agents
- Cetuximab (Erbitux) (see Cetuximab)
- Chronic Berylliosis (see Beryllium)
- Clinical
- May Present with a Sarcoidosis-Like Multisystem Disease: wheezing, etc
- Clinical
- Cytokine Release Syndrome (see Cytokine Release Syndrome): occurs with the administration of specific monoclonal antibodies
- Alemtuzumab (Campath, MabCampath, Campath-1H, Lemtrada) (see Alemtuzumab)
- Anti-Thymocyte Globulin (ATG) (see Anti-Thymocyte Globulin)
- Lenalidomide (Revlimid) (see Lenalidomide)
- Muromonab-CD3 (Orthoclone OKT3) (see Muromonab-CD3)
- Oxaliplatin (Eloxatin, Oxaliplatin Medac) (see Oxaliplatin)
- Rituximab (Rituxan) (see Anti-CD20 Therapy)
- Tisagenlecleucel (Kymriah) (see Tisagenlecleucel)
- Gemcitabine (Gemzar) (see Gemcitabine)
- Interferon-α (see Interferon)
- Mitomycin C (Mutamycin) (see Mitomycin)
- N-Acetylcysteine (Mucomyst, Acetadote, Fluimucil, Parvolex) (see N-Acetylcysteine):
- Epidemiology
- Bronchospasm Has Been Associated with Inhaled and Oral Administration
- Epidemiology
- Nitrofurantoin (Macrodantin) (see Nitrofurantoin)
- Ocrelizumab (Ocrevus) (see Ocrelizumab)
- Epidemiology
- Bronchospasm May Occur as a Manifestation of Infusion Reaction
- Epidemiology
- Opiates (see Opiates)
- Agents
- Codeine (see Codeine): codeine causes histamine release
- Fentanyl (see Fentanyl)
- Meperidine (Demerol) (see Meperidine) : meperidine causes histamine release
- Morphine (see Morphine): morphine causes histamine release
- Agents
- Paclitaxel (Taxol) (see Paclitaxel)
- Panitumumab (Vectibix) (see Panitumumab)
- Rasburicase (Elitek) (see Rasburicase)
- Ribavirin (Copegus, Moderiba, Rebetol, RibaPak, Ribasphere, RibaTab) (see Ribavirin)
- Epidemiology
- Aerosolized Ribavirin May Cause Bronchospasm
- Epidemiology
- Teniposide (Vumon) (see Teniposide)
- Trastuzumab (Herceptin) (see Trastuzumab)
- Vinblastine (Velban) (see Vinblastine)
- Zanamivir (Relenza) (see Zanamivir): inhalational
Toxin
- Acetic Acid Inhalation (see Acetic Acid)
- Ammonia Inhalation (see Ammonia)
- Bromine Inhalation/Methyl Bromide Inhalation (see Bromine-Methyl Bromide)
- Chlorine Gas/Aerosol Inhalation (see Chlorine)
- Chloropicrin Gas Inhalation (see Chloropicrin Gas)
- Cholinergic Intoxication (see Cholinergic Intoxication)
- Cigua Toxin Poisoning (see Cigua Toxin Poisoning)
- Organophosphate/Carbamate Intoxication (see Organophosphates-Carbamates)
- Scorpion Sting (see Scorpion Sting)
- Associated Scorpion Species
- Centuroides Exilicauda (Sculpuratus)
- Centuroides Suffusus
- Associated Scorpion Species
- Toxic Mushrooms (see Toxic Mushrooms)
- Associated Mushrooms
- Boletus Calopus
- Clitocybe Dealbata
- Clitocybe Illudens
- Inocybe Fastigiata
- Toxin: muscarine acts at muscarinic receptors in autonomic nervous system
- Associated Mushrooms
- Chromic Acid Inhalation (see Chromic Acid)
- Diborane Gas Inhalation (see Diborane Gas)
- Dinitrogen Tetroxide Inhalation (see Dinitrogen Tetroxide)
- Hydrofluoric Acid Inhalation (see Hydrofluoric Acid)
- Hydrogen Sulfide Gas Inhalation (see Hydrogen Sulfide Gas)
- Metal Fume Fever (see Metal Fume Fever)
- Methamphetamine (see Methamphetamine)
- Methyl Isocyanate Inhalation (see Methyl Isocyanate)
- Methyl Isothiocyanate Inhalation (see Methyl Isothiocyanate)
- Neurotoxic Shellfish Inhalation (see Neurotoxic Shellfish)
- Epidemiology
- Risk of Airway Obstruction is Highest in Patients with Asthma and Chronic Lung Disease
- Physiology
- Inhalation of Aerosolized Brevetoxins
- Epidemiology
- Nitric Acid Inhalation (see Nitric Acid)
- Nitrogen Dioxide Inhalation (see Nitrogen Dioxide)
- Ozone Inhalation (see Ozone)
- Phosgene Gas Inhalation (see Phosgene Gas)
- Phosphine Gas Inhalation (see Phosphine Gas)
- Polymer Fume Fever (see Polymer Fume Fever)
- Smoke Inhalation (see Smoke Inhalation)
- Sulfur Dioxide Inhalation (see Sulfur Dioxide)
- Sulfuric Acid Inhalation (see Sulfuric Acid)
- Sulfur Mustard Gas Inhalation (see Sulfur Mustard Gas)
- Tear Gas Inhalation (see Tear Gas)
- VX Nerve Agent (see VX Nerve Agent)
- Zinc Chloride Gas Inhalation (Smoke Bomb Exposure) (see Zinc Chloride Gas)
Pulmonary Infiltrates with Eosinophilia (PIE) Syndrome (see Pulmonary Infiltrates with Eosinophilia)
- Acute Eosinophilic Pneumonia (see Acute Eosinophilic Pneumonia)
- Acute Lung Transplant Rejection (Acute Cellular Lung Transplant Rejection) (see Acute Lung Transplant Rejection)
- Peripheral Eosinophilia May Occur with/without Pulmonary Infiltrates (as Acute Rejection May Be Detected by Surveillance Bronchoscopy with Transbronchial Biopsy Prior to the Development of Pulmonary Infiltrates)
- Allergic Bronchopulmonary Aspergillosis (ABPA) (see Allergic Bronchopulmonary Aspergillosis)
- Allergic Bronchopulmonary Candidiasis (see Candida)
- Bronchocentric Granulomatosis (see Bronchocentric Granulomatosis)
- Chronic Eosinophilic Pneumonia (see Chronic Eosinophilic Pneumonia)
- Dirofilariasis (see Dirofilariasis)
- Drug-Induced Pulmonary Eosinophilia (see Drug-Induced Pulmonary Eosinophilia)
- Eosinophilia-Myalgia Syndrome (see Eosinophilia-Myalgia Syndrome)
- Eosinophilic Granulomatosis with Polyangiitis (EGPA, Churg-Strauss Syndrome, Allergic Angiitis and Granulomatosis) (see Eosinophilic Granulomatosis with Polyangiitis)
- Hypereosinophilic Syndrome (see Hypereosinophilic Syndrome)
- Sarcoidosis (see Sarcoidosis)
- Simple Pulmonary Eosinophilia (Loffler’s Syndrome) (see Simple Pulmonary Eosinophilia)
- Tropical Pulmonary Eosinophilia (Occult Filariasis) (see Tropical Pulmonary Eosinophilia)
- Visceral Larva Migrans (see Visceral Larva Migrans)
- Other Infections
- Brucellosis (see Brucellosis)
- Coccidioidomycosis (see Coccidioidomycosis)
- Cryptococcosis (see Cryptococcosis)
- Echinococcosis (see Echinococcosis)
- Histoplasmosis (see Histoplasmosis)
- Human Immunodeficiency Virus (HIV) (see Human Immunodeficiency Virus)
- Mycobacterium Simiae (see Mycobacterium Simiae)
- Paragonimiasis (see Paragonimiasis)
- Schistosomiasis (see Schistosomiasis)
- Trichinosis (see Trichinosis)
- Tuberculosis (see Tuberculosis)
Bronchiolitis Syndrome
- Bronchiolitis (see Bronchiolitis)
- Bronchiolitis Obliterans (BO) (see Bronchiolitis Obliterans)
- Follicular Bronchiolitis (see Follicular Bronchiolitis)
- Diffuse Panbronchiolitis (see Diffuse Panbronchiolitis)
Other
- Acute Pulmonary Embolism (PE) (see Acute Pulmonary Embolism)
- Air Embolism (see Air Embolism)
- Airway Foreign Body (see Airway Foreign Body)
- Alpha-1 Antitrypsin Deficiency (see Alpha-1 Antitrypsin Deficiency)
- Anaphylaxis (see Anaphylaxis)
- Asthma (see Asthma)
- Beta Thalassemia Major (see Thalassemias)
- Epidemiology
- Small Airway Obstructive Airway Defects May Occur (for Unclear Reasons)
- Diagnosis
- Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests): PFT defects correct with transfusion and do not correlate with the iron burden, blood counts, or the degree of hemolysis
- Epidemiology
- Bronchiectasis (see Bronchiectasis)
- Byssinosis (see Byssinosis)
- Cardiac Asthma (see Congestive Heart Failure)
- Chronic Granulomatous Disease (CGD) (see Chronic Granulomatous Disease)
- Chronic Obstructive Pulmonary Disease (COPD) (see Chronic Obstructive Pulmonary Disease)
- Combined Pulmonary Fibrosis and Emphysema (see Combined Pulmonary Fibrosis and Emphysema)
- Common Variable Immunodeficiency (CVID) (see Common Variable Immunodeficiency)
- Cystic Fibrosis (CF) (see Cystic Fibrosis)
- Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia (DIPNECH) (see Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia)
- Fabry Disease (see Fabry Disease)
- Foreign Body Granulomatosis (see Foreign Body Granulomatosis)
- Hypocalcemia (see Hypocalcemia)
- Isolated IgA Deficiency (see Isolated IgA Deficiency)
- Langerhans Cell Histiocytosis (see Langerhans Cell Histiocytosis)
- Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- Earlier Nodular Disease: Normal PFT’s or Restrictive PFT’s with Decreased DLCO
- Later Cystic Disease: Obstruction (with Possible Bronchodilator Responsiveness) and Hyperinflation
- Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- Lymphangioleiomyomatosis (LAM) (see Lymphangioleiomyomatosis)
- Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- Normal: 57% of cases
- Obstructive Pattern (see Obstructive Lung Disease): 34% of cases
- Mixed Pattern: 9% of cases
- Bronchodilator Responsiveness (β2 Agonists or Muscarinic Antagonists): 30% of cases (those with bronchodilator responsiveness have a lower baseline FEV1)
- Hyperinflation with Increased TLC: common
- Gas Trapping with Increased RV and RV/TLC Ratio: common
- Decreased DLCO (Although May Be Increased During Episodes of Diffuse Alveolar Hemorrhage)
- Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- Marfan Syndrome (see Marfan Syndrome)
- Microscopic Polyangiitis (see Microscopic Polyangiitis)
- Mineral Dust Airway Disease
- Occupational Asthma (see Asthma-Occupational)
- Post-Infection Obstructive Airways Disease
- Primary Ciliary Dyskinesia (see Primary Ciliary Dyskinesia)
- Reactive Airway Dysfunction Syndrome (RADS) (see Reactive Airway Dysfunction Syndrome)
- Selective IgG Subclass Deficiency (see Selective IgG Subclass Deficiency)
- Sjogren’s Syndrome (see Sjogrens Syndrome)
- Swyer-James-Macleod Syndrome (see Swyer-James-Macleod Syndrome)
- Tuberous Sclerosis (see Tuberous Sclerosis)
- Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests): Obstruction with Decreased DLCO and Preserved Lung Volumes
Diagnosis
Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- xxxx

Clinical Manifestations
Pulmonary Manifestations
References
Etiology
- Assessment of upper airway anatomy in awake, sedated and anaesthetised patients using magnetic resonance imaging. Anaesth Intensive Care. 1994;22(2):165 [MEDLINE]
- Endobronchial nocardiosis. Eur Respir J. 1994 Oct;7(10):1903-5. doi: 10.1183/09031936.94.07101903 [MEDLINE]
- Magnetic resonance imaging of the upper airway. Effects of propofol anesthesia and nasal continuous positive airway pressure in humans. Anesthesiology. 1996;84(2):273 [MEDLINE]
- Peritonsillar abscess and infectious mononucleosis: an association or a different presentation of the same condition. Ir Med J. 1999;92(2):278 [MEDLINE]
- Endobronchial actinomycosis associated with foreign body: four cases and a review of the literature. Chest. 2002 Jun;121(6):2069-72. doi: 10.1378/chest.121.6.2069 [MEDLINE]
- Endobronchial pulmonary nocardiosis. Mt Sinai J Med. 2006 May;73(3):617-9 [MEDLINE]
